Playlist
Show Playlist
Hide Playlist
Nerve Injuries
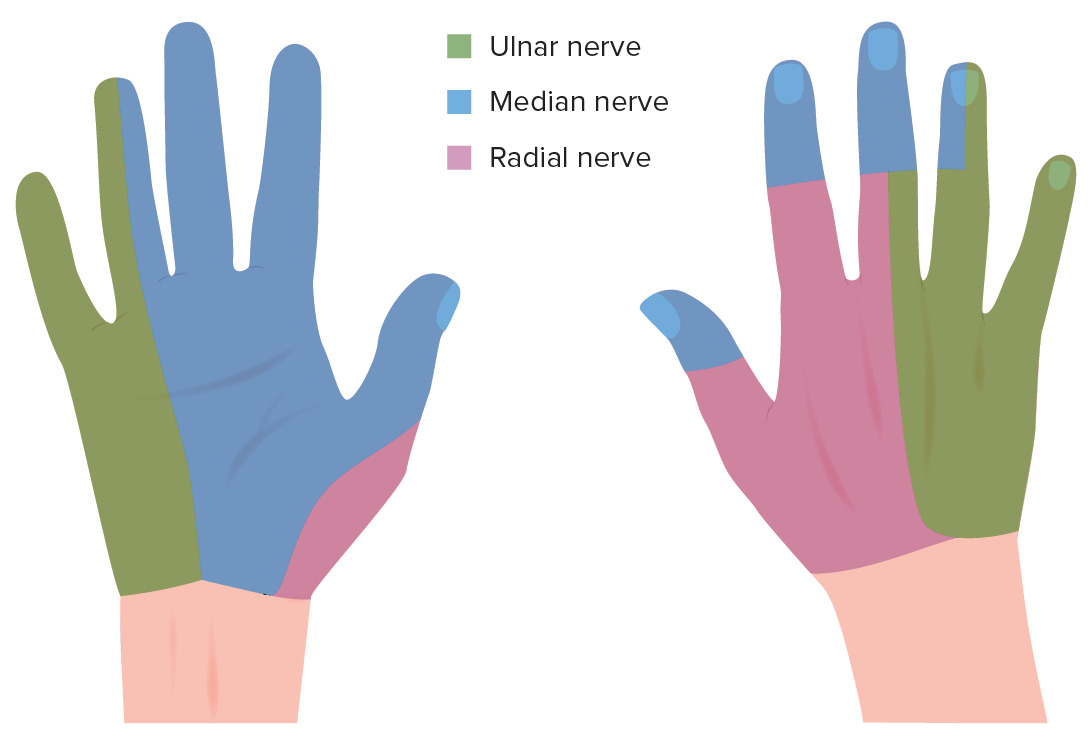
00:00 can because it’s coming out attaching on the lesser tubercle. Okay. Now, we briefly touched upon the nerve injuries. I’ll just go back to other nerve injuries you can get. 00:14 Median nerve injury. So the median nerve, as the name says, it’s like the middle. That’s what we call median. Imagine a median nerve is injured there, what do you think the patient’s clinical presentation will be? That’s the median nerve. When do you think if somebody can get a median nerve injury at this level, what’s the most common thing? Fracture. 00:49 Supracondylar fracture, commonly seen in children, but, of course, you can get in adults. 00:54 But you have supracondylar fracture; the nerve that is injured is median nerve. Of course you can get the radial nerve, ulnar nerve, in theory, but for the purpose of your exam, they’ll ask you median nerve, supracondylar fracture. So, let’s say this is a four-year-old child. He doesn’t look four, but he’s four. Supracondylar fracture, what do you think this hand will be? What are things he won’t be able to do? Wrist drop? No, no, no, wrist drop is on the other side, it's on the radial. We’re talking about median. 01:27 So, unable to extend the wrist. Flex you mean? Flex the wrist. Okay. I think I’m just working you towards a clinical scenario. They won’t give you that. What is the thing they will give you? What does the patient unable to do if it is a child? What does a classical thing a child will be laying if you’re seeing a child in any -- Grasp. The grasp. Okay. Grasp is lost. It’s called the pointing index, the index finger won’t flex. So if you see a four-year-old child laying in any, this is a classical median nerve injury. That’s called the pointing index sign. Now, in a child, you can’t ask him to make a fist. So that’s why it is in that position. But in an adult, if they are laying this, you ask them to make a fist, again, they won’t be able to make a fist but the hand will try to flex this way. 02:22 That’s called the hand of benediction. So this is again a median nerve injury. 02:28 So if we have a median nerve injury at that level, or even slightly lower down, you will soon get this pointing index or the hand of benediction. Okay. Now, let’s go to the anatomy of that. Why do you get this? Going back to your ulnar nerve, I said these two are supplied by ulnar nerve, and these two are by median. So that’s why when you have a median nerve injury, these two don’t flex. But classically, the middle finger can occasionally be supplied by the ulnar from there or the tendon is just pulling it down. But this finger will never flex. So this is the classical one but you can get this as well. 03:16 FPL, even this one flex because the FPL is also by the median nerve. If you come to the carpal tunnel and you have an injury of the median nerve at this level, then you won’t get pointing index, you won’t get hand of benediction, what is lost? Thenar, I mean wasting of thenar, but what does a patient unable to do? Abduction. Abduction of thumb. So that is lost in the median nerve injury. Well, clearly, if it happens there, it will definitely be lost. 03:50 But if the patient has got a full fist but unable to just abduct the thumb then it’s the median nerve lower than the carpal tunnel. Okay. So these are the levels of median nerve injury that they will ask you. Ulnar nerve injury. Ulnar nerve injury, they’ll ask you whether it can be -- before the epicondyle or after. If you have an ulnar nerve injury at this level, what will you get? What will the patient sign, acutely and chronically? You get a drop. No, you won’t. In the chronic situation, you’ll get clawing of the hand. Acutely, what is the patient unable to do? These two fingers, isn’t it? So if the patient makes a fist, these won’t flex, these two. 04:51 But with the long standing ulnar nerve injury, you will get wasting of the hypothenar eminence, claw hand. Now, in your exam, what are the other things they will expect you to know about ulnar nerve in the hand? What are the functions of ulnar nerve in the hand? Jay-P, what are the other functions of ulnar nerve in the hand? What are things you can ask the patient to do to check for ulnar nerve intactness? Flexion of the medial two digits. Okay. So you can ask them to make a fist, fine, that may be lost, what else? Very good, spreading the fingers. So that is abduction of the fingers, adduction of the fingers, as well as scissoring. Then adduction of the thumb and then abduction of the little finger. All of these are for ulnar nerve injury. So if we have somebody with an ulnar nerve injury -- so that is lost in ulnar nerve injury. Then you do the Froment’s sign, which is giving your card between the thumb and index finger, and then you pull the card out. 06:17 So if the patient has got an ulnar nerve injury, the adductor pollicis is affected and the patient will be unable to hold the card but they will try to hold the card by flexing the IP joint. Your finger is in that position. That’s your positive Froment’s sign. That’s the classical of ulnar nerve injury and you’re testing for adductor pollicis. Okay. Back to you. What’s the mechanism of claw hand? So if it’s a proximal injury, you get a claw hand and if it’s distally, you don't because you got a compensation. It’s because if it's a proximal injury, you get -- Well, maybe I should just correct you there. You will get a claw hand in both. Both in high lesion as well as low lesion, you’ll get a claw hand, but there’s a difference. 07:26 What’s the principle behind the claw hand? What’s claw hand? Show me how does claw hand look. No. 07:37 How do you distinguish a claw hand from Dupuytren's contracture or the Volkmann's contracture? Okay. No, just by looking at it. In a claw hand, the classical feature is hyperextension of the MCP joint and flexion of the IP joint. 07:53 So this is claw hand. These two joints have to be hyperextended. That’s claw hand, because if you get this, then you’re getting a number of conditions. You can get Dupuytren's bone contracture, Volkmann’s contracture, etc. But in a claw hand, that’s claw hand. So, that brings us to the muscles in the hand. To understand claw hand, you need to understand action of muscles. I said this action, abduction of the fingers. That is by, what interossei? Palmar or dorsal? Palmar. 08:31 Dorsal, DAB. PAD AND DAB isn’t it? DAB is dorsal interossei. So dorsal interossei abducts, palmar interossei adducts. So there are four and four, so eight muscles. Then you have four hypothenar muscles, four thenar muscles. So that’s 16, and finally, your lumbricals. 09:02 What is the action of lumbricals? This is the action of lumbricals. That’s when you put somebody on a plastic cast, you put them in this position. Because in your normal resting position of the hand, the lumbricals will help in flexion of the MCP and extension of the interphalangeal joints. That’s the lumbrical action. 09:23 Now, spread your fingers, that’s all ulnar nerve, bring it together, all ulnar nerve. 09:40 What about that? Which nerve is this? Radial? Extension of the -- No, this action. Median and ulnar. 09:50 Very good, yes. So these two are by ulnar and these two are by median. I will explain that bit of anatomy now. In the hand, we discuss about 20 muscles, four thenar, four hypothenar, four palmar interossei, four dorsal interossei, and four lumbricals. All these are supplied by the ulnar nerve except those on the radial site which are called the LOAF muscles. 10:28 So the LOAF is supplied by the median nerve. L stands for lateral to lumbricals, opponens pollicis, abductor pollicis brevis, and flexor pollicis brevis. These four are supplied -- well, these four means these five, the lateral two lumbricals; opponens pollicis, abductor pollicis brevis, and flexor pollicis. These are supplied by the median nerve. Everything else is by ulnar. So this action, these two are by median, these two are by ulnar. So, what happens? If you have an ulnar nerve injury, these two are spared. That’s where you get the clawing. So what happens in clawing? If you have your hand in this position, when you have a nerve injury, the opposite of that happens. 11:19 So, the opposite will be hyperextension of the MCP and flexion of the interphalangeal joint. 11:27 These two are not affected. It will get clawing only in those two. This is your claw hand. 11:34 Now, what you said was high lesion and low lesion. If you have a high ulnar nerve injury, then these two FDPs are also affected on there because the FDP is supplied by ulnar nerve quite higher up here. So your clawing will be less because they’re also affected. 11:55 The hand is clawed less. But if there’s a low injury, this nerve is intact, so it's pulling it more. Okay. So that is your ulnar nerve paradox. If you have a high lesion, the clawing is less. If you have a low lesion here, the clawing is more. That’s your ulnar nerve injury, ulnar nerve paradox. So if you got anything related to this in your EMQs, usually, high lesion, low lesion. They like high lesion for ulnar nerve and radial nerve because it’s got quite a bit of clinical significance. Did you understand the clawing concepts, and the high lesion and the low lesion? Okay. So that’s all you need to know about the hand. At this level, you don’t have to know about the arches. 12:46 You don’t have to know about the pulley system or the other detailed anatomy. If you want to ask me anything at this point of what you’re wasting in other MCQs, if you want to ask me anything at this point, I can answer you but I’m not going to any more detailed high anatomy because that will be too much for you. 13:07 Is anybody wanting to know about pulleys? No, I don’t think so. You need to know where is the insertion of the FDP and FDS. Where does the FDP insert, flexor digitorum profundus insert? Base of the distal phalanx. And FDS? No, because the FDS has got two strands coming off. So the FDP and FDS comes here. FDS splits into two. It’s called the Camper’s chiasm, and it’s attached to the sides of the middle phalanx. The FDP comes to the middle and attaches to the distal phalanx. That’s your FDP and FDS insertion. 14:13 Okay. The last bit here is the carpal tunnel, extremely important. Attachments of the flexor retinaculum. Do you want to say that? Attachment, yup. Anyone, attachments of the flexor retinaculum. 14:31 Scaphoid? Scaphoid, on the radial side, okay. 14:40 Trapezium. Trapezium, pisiform, and what’s the bony figure in your hand? Probably lunate? Oh no, hamate, hook of hamate. Okay. Something like the flexor retinaculum, you need to know the attachments because it’s quite an important thing in the exam. This is your flexor retinaculum. 15:14 The proximal part of your flexor retinaculum is your distal wrist crease. If you see your distal wrist crease in your hand, that is the proximal part of the retinaculum. 15:24 Then if you ask a patient to extend the thumb fully, extend it fully, then the ulnar border of the thumb forms the distal part of the retinaculum. You extend it fully then identify the ulnar border of the thumb. That’s your distal part of the retinaculum. So this is your retinaculum. 15:46 The attachment here is the tubercle of the scaphoid. Just remember that the carpal bones are in a concave shape such that the retinaculum does not attach to the entire bone. It just attach to specific points. So on the scaphoid, it’s called the tubercle of the scaphoid. 16:08 Pisiform. The pisiform is a small bone so it attaches to the pisiform. Here, it is a hook of the hamate, not the entire hamate, hook of the hamate. And here, it’s a ridge of the trapezium. So this is where the attachment is. 16:26 So if you feel the bony prominence here, that is your hook of hamate. Okay. Structures going under the retinaculum, this is very important. So you have the median nerve then you have the FDP and FDS to this finger, so eight of them, and FPL. So ten structures. Ten structures go under the retinaculum, and what goes over the retinaculum? Anyone? You know what, the flexor carpi ulnaris, what did you say, is that radialis? No. You know, some of the books do say that but it’s not strictly accurate. The flexor carpi radialis, does not go under or over the retinaculum because it just attaches to the base of the second metacarpal. 17:18 So it has nothing to do with the retinaculum. Yeah, palmaris longus goes over the retinaculum. 17:24 What else? Ulnar nerve, ulnar artery, anything else? If you have a patient coming with carpal tunnel, carpal tunnel syndrome, what is it classically feature? They’ll have tingling and numbness in the lateral three digits, right? If you test for sensation, can that be affected? It can be. But what about sensation here, can it be affected? No. Why not? Radial nerve. No. Here. It’s a branch. 18:04 Once it comes up before the -- That’s right. Okay. So, that’s the median nerve. Approximately five centimeters before the wrist crease, there is a branch called the palmar cutaneous branch of the median nerve, which supplies the thenar eminence. 18:28 So if we have a patient with carpal tunnel, because this is running over the retinaculum, that area is spared. How it work? After you operate and see them postoperatively, you need to test this because if that is lost, then you have iatrogenically damaged the palmar cutaneous branch. Okay. What is radial artery? The radial artery comes here just lateral to your FCR tendon. The deep branch goes to the snuffbox, and then it comes out through the thenar eminence to form the palmar arch. But you have a superficial branch which goes over the retinaculum, and anastomosis with the ulnar artery and other side to form the other part of the palmar arch. Essentially, you have a superficial branch of the radial artery, palmar cutaneous branch of the median nerve, palmaris longus, ulnar nerve, ulnar artery. So these are all structures going over the retinaculum. Okay. So, we have covered the entire upper limb on this. Couple of nerves we haven’t covered, one is the long thoracic nerve which comes from C5, C6, and C7. So, root value is C5, C6, C7. It lies in the midaxillary line in the chest or the thorax, and it can be damaged when you put in a chest drain or do any surgery in the axillary region. So that’s the long thoracic. Then a couple of more nerves just for completion, we have the nerve to subclavius from there and the nerve to rhomboid. But I don’t think you need to know for the part A, you just need to -- if at all you’re asked, you just need to get in your head that it has nothing to do with the cords. It is just an isolated nerve coming off the root, nerve to subclavius and the nerve to rhomboid. Okay. I think that pretty much covers everything. 20:40 We are spot on time. What I’m going to do is go through the slides. As I said, all these slides are going to be available for you online. So you don’t have to worry. The purpose of going to the slides is just to reinforce what you have learned and for you to just have a quick revision. Okay. I’ll come to the axillary artery when we do the thorax and axilla as well. The shoulder joint, a lot of theory. I haven't cover
About the Lecture
The lecture Nerve Injuries by Stuart Enoch, PhD is from the course Musculoskeletal - Upper Limb.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Loved these lectures. The ONLY thing that bothered me was that the heads of the audience kept blocking exactly the subject's hand during the demonstration. Other than that, great job!