Playlist
Show Playlist
Hide Playlist
Myocarditis: Manifestations, Signs and Symptoms, Diagnostics, and Management
-
Slides Myocarditis Pericarditis.pdf
-
Reference List Pathology.pdf
-
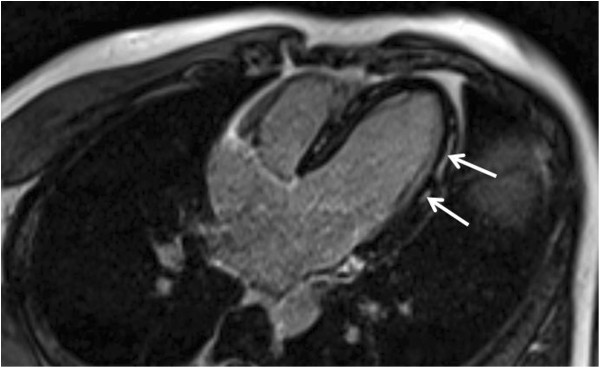
Download Lecture Overview
00:01 So, let's come back to COVID. And I said, you know, earlier it's really probably not a cause of myocarditis. So fact or fiction? A very small percentage of patients who developed COVID overall developed some degree of cardiac decompensation. So a lot of people potentially infected, not all of them are symptomatic. If you take all comers, there's very little incidence of cardiac decompensation. Clearly, cardiac decompensation is much more common in fatal cases but this in fact is certainly multifactorial. In fact, when we look at the histology of fatal cases of COVID-associated myocarditis we don't see myocarditis, we don't see a lymphocyte and macrophage-rich infiltrate. Rather what we see is microvascular infaraction. And in fact, we know for a fact that in COVID we get a hypercoagulable state and we are also stressing these patients, they are hypoxic so you have increased catecols, a combination of vasospasm and increased hypercoagulability causes microvascular thrombosis and then we're getting microvascular infarction but it is not myocarditis. Take it from me. There has also been reports of increased incidence of Kawasaki's vasculitis so you may recall from having listened to the vasculitis talk that we had at some other point and Kawasaki's disease, Kawasaki vasculitis is associated with a variety of viral infections in kids and one of the most feared complications is a vasculitis involving the coronary arteries. There had been a report of increased incidence of this particular entity in kids who got COVID. This does not appear to be the case. So, fact or fiction, you can tell your friends now "Nah, there is not really a COVID-associated myocarditis, there are cardiac complications and manifestations but it is not a primary infection of the heart. Okay, what manifestations of myocarditis can we see? So you can have an absent or minimal symptoms. So this is really subclinical. You can have acute disease where heart failure develops in less than 3 months at relatively rapid phase. We can have heart failure that develops over greater than 3 months. So there are a whole variety of kind of temporal sequencing of what can happen once you have inflammation in the heart. Signs and symptoms are related to myocardial dysfunction. These patients will have dyspnea and orthopnea that's due to left heart failure. They may have chest pain or tachycardia depending whether the inflammation is affecting the pericardial nerves and causing then firing of those. They may have arrhythmias because we are destroying individual myocytes and we therefore may have not normal conduction cell to cell to cell. They may have abdominal pain. Again, this is largely related to heart failure. They may also have right-sided heart failure with distended jugular veins, jugular venous distention, indicating that the heart is not pumping well on the right side and this is another manifestation that you get systemic peripheral edema. When we are trying to diagnose this, as a laboratory test we can look for elevated troponins basically reflecting myocyte damage. And on ECG, we see a variety of very nonspecific things. So we can see a sinus tachycardia as the heart is not pumping effectively. We do see increased heart rate. We can see nonspecific ST–T wave changes. 03:41 So the repolarization because of the myocyte injury is abnormal, but it's in a nonspecific pattern. And we can see a variety of arrhythmias from atrial fibrillation to supraventricular tachycardia to heart block depending on where the inflammation is occurring within the myocardium. On MRI or echocardiogram imaging, on MRI you may see an increased signalling for inflammation and on echocardiogram you're going to see diminished contractility. But again, this can be somewhat nonspecific. And then finally, the gold standard for diagnosing myocarditis is not the clinical diagnostics that I've just mentioned, but it's endomyocardial biopsy going in, taking some snippets of the heart and sending it off to your friendly cardiac pathologist. And with that, we'll conclude our discussion of myocarditis.
About the Lecture
The lecture Myocarditis: Manifestations, Signs and Symptoms, Diagnostics, and Management by Richard Mitchell, MD, PhD is from the course Myocarditis and Pericarditis.
Included Quiz Questions
What defines chronic myocarditis?
- Heart failure developing later than three months after the disease begins
- Heart failure lasting more than three months
- Heart failure lasting more than six months
- Heart failure developing later than six months after the disease begins
- Heart failure lasting more than one year
What is the gold standard for the diagnosis of myocarditis?
- Endomyocardial biopsy
- Elevated troponins
- Jugular venous distention on physical examination
- Sinus tachycardia
- Identification of infectious etiology (e.g., Lyme disease)
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |