Playlist
Show Playlist
Hide Playlist
Myocardial Infarct: Tissue Patterns and Cellular Injuries
-
Slides Complications of Atherosclerosis.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
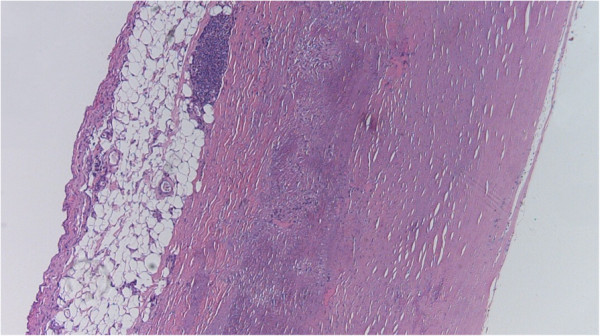
00:01 Let's talk about the patterns of infarct in the heart. 00:03 And it's not just one glob of muscle, they're in fact as you know, their structure, there's a right ventricle, there's left ventricle and there's different circulations. 00:13 So the patterns of infarct in the heart will depend on the circulation around the heart. 00:19 So on the left hand side, we're looking at transmural infarcts. 00:23 And we're looking at the various distributions depending on which vessel is occluded. 00:28 Transmural infarcts literally means the entire thickness of the wall has infarcted. 00:35 In parentheses, in passing, there is always a little tiny rim, maybe 5-6 myocytes thick at the endocardial surface that are still viable, even in a transmural infarct. 00:49 That's because that lumen of the ventricle has got some oxygenated blood in it, and that that layer of 7-8 myocytes, gets its oxygen, nutrition whatever it needs from diffusion, from the lumen. 01:05 So we will always have a preserved zone, even in a transmural infarct. 01:09 Having said that, transmural infarcts are usually proximal occlusions of large vessels. 01:17 If you proximally occlude the left anterior descending, kind of the anterior septum and anterior wall of left ventricle will be infarcted. 01:30 If you occlude the left circumflex in a proximal distribution, that lateral hunk of the wall will be the area of infarct. 01:39 And if you have a large proximal occlusion of the right coronary artery, It tends to be the posterior septum and the posterior wall, and depending on where it is, you may also have parts of the right ventricle that are also infarcted. 01:53 So those are transmural infarcts, and they're usually large plaque, large vessels with a plaque rupture and a complete thrombus. 02:03 Now you can also have non transmural, so-called subendocardial myocyte infarctions. 02:09 And this has to do with the fact that blood supply comes from the surface epicardial vessels, percolates through the myocardium and then the last part of the heart to get its blood supply is that zone nearest the ventricle, ventricle lumen. 02:24 So that's a subendocardial myocardial infarction - SEMI, okay. 02:30 And that is a non-transmural infarct. 02:33 What that means is that we have limiting supply but it's not complete cut-off of supply. 02:41 So only the tissues that get the blood supplied last are the ones not getting enough oxygen or not getting enough nutrition, and they're the ones that die. 02:51 So this is a partial obstruction say of the left anterior descending. 02:55 This is the first image at the top there on the right. 02:57 We have a partial obstruction, we have limiting flow to begin with and then we make the patient overall hypoxic, we increase demand. 03:09 We have some blood loss someplace and now that... 03:15 somewhat limiting flow in that vessel now becomes sufficiently diminished that we kill off the subendocardial zone. 03:25 And then, that could be played out as a left circumflex subpartial obstruction or a right coronary subpartial obstruction. 03:35 If you have three vessel disease as indicated in this next image in the middle on the right hand side, so you have limiting flow to all three and then you have global hypotension. 03:47 Or you have blood loss or you have hypoxia or you have anemia, that limiting flow can actually, in all three vessels, give you a global, circumferential subendocardial infarct all the way around the inside of the heart. 04:04 There's one other pattern that you should be aware of. 04:07 So these are larger vessels, but sometimes smaller intramural vessels become occluded for a variety of reasons, and then you can get scattered microinfarcts throughout the left ventricle. 04:19 These small intramural vessel occlusions can occur because of a vegetation on a valve that flips off little tiny emboli into the vessels. 04:27 It can be due to vasculitis that's in the vessels of a myocardium where we have inflammation and then thrombosis in small vessels. 04:35 It can be due to microvascular spasm. 04:39 So a number of drugs - cocaine, for example, can cause vessels to squeeze in a very kind of random pattern and that squeezing the vessels if it lasts for 20 to 30 minutes, that little area of myocardium is going to die. 04:53 When you hear about people being scared to death, that's actually a real thing. 04:59 What happens is the epinephrine release by the adrenal medulla is actually causing vasospasm of small arteries within the heart, and we're getting microvascular infarcts. 05:11 Now that can either lead to arrhythmias, or it can actually lead to enough dysfunction that the patient doesn't squeeze their myocardium effectively, and it will have that pattern of scattered microvascular infarction. 05:25 All of this can be modified somewhat by the restoration of flow. 05:29 Remember that up to about an hour the endothelium is probably okay, but after an hour that endothelium is starting to die. 05:38 So if we have infarcted myocardium and then we restore blood flow after an hour of no flow, we will restore blood into tissues and it will bleed. 05:50 So we will have a hemorrhagic infarct superimposed on just the necrosis of the myocardium. 05:58 All right, how do we recognize this as students and as pathologists? So let's think about this. 06:06 We have, infarct at time 0. 06:09 so we're looking at various effects on the y axis and the duration of injury on the x axis Time 0, we start infarcting the heart or we cut off the blood supply. 06:22 It's not yet dead, but the cell function goes down dramatically very quickly within a couple of minutes, we are no longer contracting. 06:30 The cells are no longer squeezing. 06:32 So that partial portion of the heart is at standstill. 06:35 So the cell function is lost very, very quickly, but up to about 20 to 30 minutes, we can reverse that. 06:43 If we jump in there and restore blood flow, everything will be okay, nothing will have died. 06:48 So we're at reversible cell injury in that first green box However, as time progresses and the duration of the ischemia, the duration of the hypoxia, the duration of the loss of nutrition continues, we will reach a point of no return. 07:06 And that's when we get cell death, so that's starting to come up at beginning about 20 to 30 to 40 minutes. 07:13 But we can't really recognize that. 07:15 Clearly as pathologist at the autopsy table, we will have a dead person, but the myocardium to us at that early time point may look completely normal. 07:25 What we will find is a completely occluded coronary artery and we say, 'yeah, patient died as a result of a thrombosis and infarct, myocardial infarct'. 07:36 Beginning a little bit later after that cell death is things that we, as pathologist you as students of pathology looking down the microscope can identify. 07:46 And the ultra structural changes that is to say by electron microscopy is going to be the next thing that will occur and we can identify those as probably the earliest morphologic changes that will occur after an infarct. 08:01 By light microscopy, so the traditional hematoxylin-eosin staining, the H and E stain, we will begin to see that those changes at about 12 to 24 hours and we'll show you pictures in subsequent slides And grossly at the autopsy table, we'll be able to recognize the gross morphologic changes. 08:21 Aht about a couple, 3 days I can look at a heart that's been infarcted. 08:26 And if the patient had survived for a sufficiently long periods of time up to about 2 to 3 days, I can go, 'Oh yeah, that area is dead', particularly if there's been reperfusion, I can say, 'Yeah, that's dead and it got reperfused because there's hemorrhage there as well'. 08:40 Okay, so injury, reversible injury precedes irreversible - yeah, I've got that. 08:45 But then the way that we can perceive it also occurs in kind of waves, subsequent waves after that.
About the Lecture
The lecture Myocardial Infarct: Tissue Patterns and Cellular Injuries by Richard Mitchell, MD, PhD is from the course Atherosclerosis.
Included Quiz Questions
Transmural infarcts are commonly seen in...
- ...proximal occlusion of large vessels.
- ...distal occlusion of large vessels.
- ...partial occlusion of large vessels.
- ...complete occlusion of small vessels.
- ...partial occlusion of small vessels.
Permanent occlusion of the right coronary artery results in the infarction of ...
- ...the inferior region.
- ...the anterior wall.
- ...the medial wall.
- ...the lateral wall.
What do small intramural vessel occlusions cause?
- Scattered microinfarct
- Circumferential subendocardial infarct
- Regional subendocardial infarct
- Proximal occlusion of large vessels
- Large transmural infarct
The effects of myocardial cell injury can be reversed up to...
- ...30 minutes.
- ...60 minutes.
- ...1–4 hours.
- ...12–24 hours.
- ...3 days.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |