Playlist
Show Playlist
Hide Playlist
Molecular Basis of Cancer
-
Slides CP Neoplasia Definitions.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
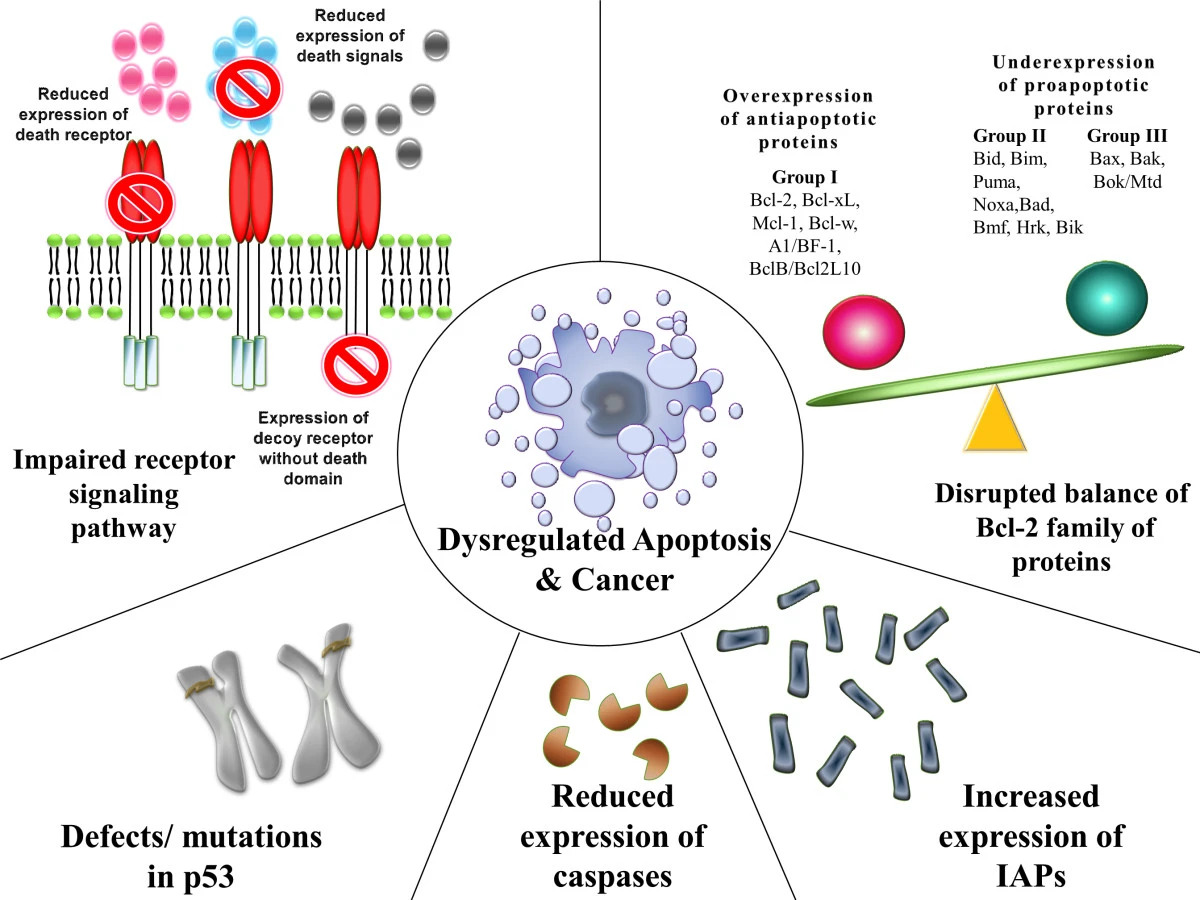
00:00 So, how does this happen? How does a good cell go bad? So even normal cell and it's subject to the various vicissitudes of life, we're all being bombarded by chemicals from radiation, viruses, and other things that are potentially carcinogenic. And the normal cell gets injured. The normal nuclear material, the genome is injured. There is DNA damage. 00:27 But in the vast majority of the rest and the vast majority of the time, we have mechanisms to recognize the damaged DNA and to fix it so we have successful repair or back to normal cell even though it was, at one point, injured. Now sometimes though, however, you can have failure of that DNA repair mechanism. Now you may have so much damage that the cell can't possibly repair at all, but you can also have defects that occur in the setting of inherited mutations in the ability to do DNA repair. We'll talk more about those, but there are certain syndromes that are responsible for failure of DNA repair and the BRCA1 gene, if you inherit that particular gene your ability to repair DNA is diminished and that's why those patients have higher risk of breast and GU malignancies. You can also have genes that affect the growth of a cell, so proto-oncogenes, or affect apoptosis. So if a cell doesn't die when there's DNA damage, normally a cell that gets too much DNA damage kills itself and undergoes apoptosis. There are normal pathways for that. But if we turn off the apoptosis pathways, then the cell won't kill itself appropriately. So those are inherited mutations that can impact the DNA repair mechanisms. So, if we don't adequately and accurately repair DNA damage, then we will accumulate mutations in the genome or the somatic cells. Now, some of those will beat silent mutations. Some of those will not have any impact at all, but others can drive an ongoing proliferation. So mutations in the genome of the somatic cells can potentially now, in the green box, cause activation of growth promoting oncogenes. So oncogenes just mean genes that normally regulate cell proliferation, they're not really there because they're cancer genes but if we turn them on they become cancer drivers. So you can, because of the mutations in the genome, have increased activity or increased amounts of growth-promoting oncogenes. 02:47 Alternatively, you can have inactivation of tumor suppressor genes. Because as we've evolved over time, the cells know that there is the potential to acquire proliferation that is due to mutations and so there are variety of genes very importantly that inhibit normal proliferation. It's a very tightly tuned set of mechanisms in normal cells. There is normal turnover and there is normal suppression of that turnover. So if we inactivate tumor suppressor genes, you will have as profound an affect as activating growth promoting oncogenes. Okay. And then if either of those happen or both happen, then we'll get unregulated cellular proliferation. Alright. That's only part of the story. It just means the cells are growing. Okay. And in fact that could be those colonic polyps that are benign. 03:43 It's still not malignant, but we're on our way. Now we have unregulated cell proliferation. 03:51 And again as I mentioned previously, normal cells are constantly turning over and at the same time they're normally dying. We have a tightly regulated amount of proliferation and death. The death that is happening is due to apoptosis. So, if we turn off the apoptotic mechanism that would normally kill a cell when its useful lifespan is over, then we will have again increased cell number. They're just not dying appropriately. So that means decreased apoptosis and unregulate cell proliferation and decreased apoptosis, again we're getting closer to malignancy but there are still a couple other steps that we have to do. That will give us a clonal expansion. Okay, on to the next slide. With the clonal expansion, again if there's genetic instability that doesn't kill the cell we will acquire additional mutations. 04:48 Okay, now we're getting closer to cancer. We clearly, as a cell population is expanding, it is outgrowing its vascular supply. The tumor is expanding but tumors are played by the regular rules of normal cells they have to have adequate vascularisation in order to live. 05:10 So, in order for a cancer to grow and continue to expand, as it gets bigger and bigger and bigger, it needs to induce antigenesis. It needs to induce avascular supply to keep up with that clonal expansion, otherwise it would only get to a certain little teeny tiny size and it couldn't get any bigger because it would effectively outstrip its ability to get oxygen and nutrition. It's also important because we're acquiring mutations. The tumor now is becoming antigenic. It's expressing new mutated proteins, for example, that the immune system can recognize so there has to be a mechanism by which these expanding cells also escape that immune surveillance mechanism. So we'll give progression, we're very close here to malignancy. Finally we crossed that Rubicon where we have a malignant neoplasm where it has acquired all other mutations necessary to now continue to grow without any exogenous stimulus. It's got enough blood supply, it's escaping the immune system, we have acquired sufficient mutations to have a recognizable malignant neoplasm. Hopefully as we gone through this, you see it's a multistep process. It's not, you know, a single bolt of lightning that hits a cell and turns it malignant, far from it. It requires many many many steps to get there. And then the malignant neoplasm can exert some of its malignant potential by invading and by metastasizing, by breaking off going into the bloodstream or lymphatics and going elsewhere within the body. See that dotted red line at the top? Well, that may refer to this again in future talks. This material that's below the red line won't be covered more today in any significant extent, but below this red line will be very important as we talk about how cancers cause death, injury, pathology in the human host that's got that cancer. For today, we're going to finish out talking about the things that came before the red line.
About the Lecture
The lecture Molecular Basis of Cancer by Richard Mitchell, MD, PhD is from the course Neoplasia.
Included Quiz Questions
What can lead to the inability to repair DNA damage?
- An inherited mutation that affects cell growth
- Exposure to chemicals
- Radiation exposure
- Active HIV infection
- CMV infection
What is one process that drives the progression from clonal expansion to tumor progression?
- Angiogenesis
- DNA repair
- Apoptosis
- A robust immune response
- Chemotherapy initiation
What is required for metastasis?
- Malignant neoplasm
- Cell proliferation
- Clonal expansion
- Cellular apoptosis
- Cell cycle arrest
Which of the following leads to clonal expansion?
- Decreased apoptosis
- Activation of tumor suppressor genes
- Regulated cell proliferation
- Inactivation of growth-promoting oncogenes
- DNA repair of mutations in the somatic genome
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |