Playlist
Show Playlist
Hide Playlist
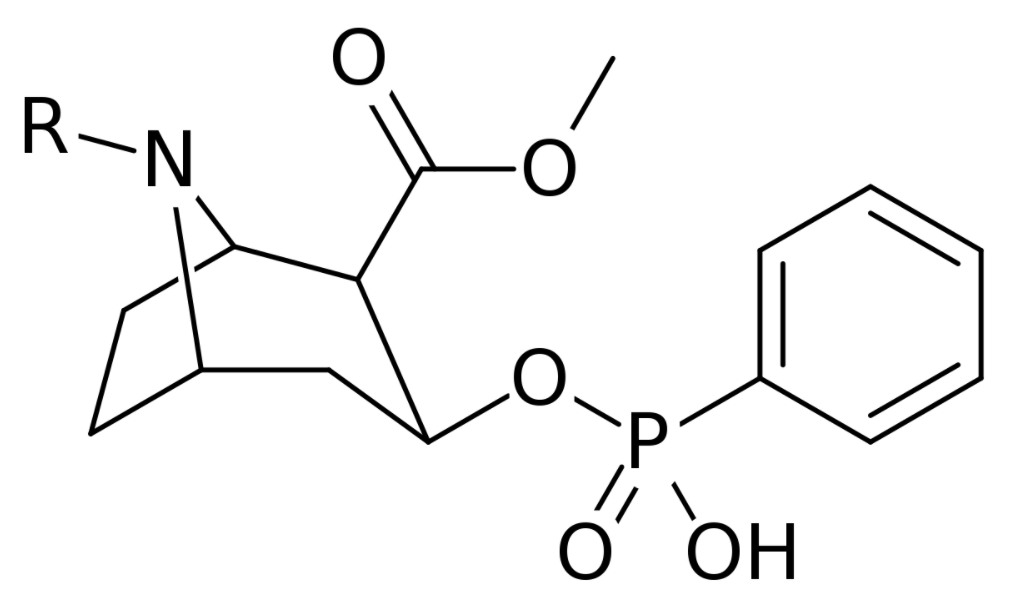
Local Anesthesia
00:00 Okay, the local anesthetic is a very favorite subject in the exam. 00:05 They have inevitably have to question somewhere in this topic. 00:15 Okay first slide, it's boring, just to give you an idea of when in your local, You know, local anesthetic for look infiltration, nerve blocks, spinals, epidural, IV administration fine. 00:28 Okay, very important this slide. 00:32 All local anesthetics contain a lipophilic aromatic group and hydrophilic groups. 00:37 So, basically fat and water. 00:40 Okay, a combination of fat. 00:44 So, I won't draw the the chemistry of this but you just think about it this way. 00:52 Fat. 00:53 Water. 00:54 They are either connected by an ester or amide. 01:01 That's it, that's the local. 01:06 So all local anesthetic contains a lipophilic aromatic group and hydrophilic group that are linked by either amide or ester. 01:14 Amide are stable and have a longer shelf of life. 01:19 Well, esters are more volatile. 01:22 Give me a some example of ester. 01:27 Sniffing. 01:27 Okay. 01:28 Okay, cooked cocaine, anything volatile is an ester. 01:33 So amides is a standard, Lidocaine, bupivacaine, prilocaine. 01:39 These are your standard amides. 01:41 So they have a longer shelf life. 01:43 Okay, and ester is got cocaine and amethocaine. 01:47 We really don't use that much on a day-to-day practice. 01:50 So you need to really know about amides. 01:53 Question has been asked about adrenaline concentration, 1 in 200,000. 01:57 Nothing less in a local anesthetic. 02:02 Okay, 1 in 200. 02:05 Okay, the important ones, llidocaine, short-acting. 02:09 How short? How many hours? When do you give patient Lidocaine? When do you do it, ask take some paracetamol after few hours. 02:19 2 to 4 hours, it maximum 2 to 4 hours Bupivacaine is slightly longer acting. 02:26 We know of the 68 hours, Bupivacaine is more cardiotoxic than Lidocaine. 02:34 Because it's more lipid soluble the hence, its safe dose of bupivacaine with or without adrenaline is the same. 02:43 Okay. 02:48 If at all they have asked about local anesthetic. 02:50 They will ask about the mechanism of faction. 02:53 And I have highlighted this because this is a statement they usually ask. 02:58 Prevent influx of calcium inhibition, potassium inhibition, sodium. 03:02 So that's all you need to remember. 03:03 It prevents sodium inhibition, inhibiting the propagation of the action potential, okay. 03:10 So this is the crucial physiology behind how a local anesthetic works. 03:16 It inhibits the influx of sodium and prevents it from giving a action potential. 03:24 Okay. 03:27 This is more of theory, but in their exam, they won't have to have the time to ask you so much theory. 03:33 It will be just one statement. 03:36 Okay, and it causes reversible blockade of motor and sensory nerves. 03:41 Potency of ALA is related to the dose and lipid solubility. 03:46 There's another MCQ question. 03:48 Dosage and how soluble it is in lipid. 03:51 I'll give an example. 03:52 Okay. 03:53 Now I'm going to spend a bit of time on this and you need to really get this right. 03:59 Calculation of the maximum dose. 04:01 You need, I'm sure you might have worked, learned about this in pharmacology. 04:06 100% of a drug, so if you have a vial of local, 100% of the drug has got one milligram per ml. 04:16 So if you get a 1 Ml ampule, if it is hundred percent concentration, that is got one gram of the drug. 04:25 Okay. 04:26 Therefore 10% concentration is 100 ml, 100 mg per ml, and 1% is 10 milligrams per ml. 04:32 This is what you need to remember. 04:47 I normally work it out at this point, 1% is 10 mg, 2% is 20 mg, .5% is 5 mg. 04:56 That's how I work it out. 04:58 But for your better understanding you can start from here. 05:02 A drug, with a hundred percent concentration has got one gram. 05:09 Per ml. 05:11 1 gram per 1 ml. 05:13 So, 1% is 10 mg per ml. 05:16 Did you get that? So if you understand that then you can work out the maximum safe dose. 05:23 So if you give with adrenaline, it limits the blood flow to the area so increases the total dosage provides a bloodless field, blanching of the skin is shown, the area of infiltration is Blanche, and clearly must not be used in any doctor is, this is standard thing which is said But nowadays, we are still given digital vessels If you feel confident and if you're working especially center then spine you you can use in and arteries but not for the for an exam. 05:58 Okay. 05:59 It's not a dose. 06:00 We remember this. 06:15 Okay, so you will be given a scenario, 70-year-old coming for extension of something. 06:22 What's the maximum safe dose of Lidocaine with adrenaline? So you need to have those values. 06:29 So this is normally we give it a 3 to 5, 5 to 7. 06:33 But in the exam, you may get it as, just keep it to 3. 06:43 Okay. 06:43 Now at this point I need to ask you, you need to know how to calculate the ml from the milligram. 06:49 So the question will be, 70 kilogram patient coming for local anesthetic. 06:55 You're giving one percent of Lidocaine, how many mil’s can give? 70-kilogram patient coming in for surgery for some surgery, and you are infiltrating 1% of Lidocaine without adrenaline without without adrenaline. 07:16 What's the volume you can give? 21 mil’s, 21 to 35 mil’s. 07:21 So 3 to 5 mil’s is 21 to 35, yeah. 07:24 If it was 2%. 07:30 10.5 average. 07:33 Okay. 07:35 So your exam will never ask you in milligram, they'll ask in milliliter, because that's what we've get in the hospital, right? We don't, we'll just get 1% Lidocaine given to us. 07:46 So you need to know how many, what's the volume you can give. 07:49 So but you need to work it out in the exam that calculation. 07:53 So remember, 1% of Lidocaine is 10 milligrams of the drug. 08:03 Okay, what about an infected sides? Can you use local? You can use but probably doesn't work. 08:09 Because infection has gotten acidotic environment and it won't penetrate the cell membrane for preventing the depolarization. 08:20 And it can also worsen cellulitis in local, so you probably don't use local anesthetic in an area of infection. 08:29 Signs of local anesthetic toxicity. 08:33 This one, circumoral tingling and paraesthesia, unconsciousness, coma, cardiac disturbances. 08:41 And I put up this slide because it's the normal questions it's been asked what they give. 08:46 The reason I put up with this, I never come across this lipid emulsion, but I've read in many books about this. 08:52 This is a standard management. 08:54 I don't know whether the hospital has it, but they say if you have toxicity you need to stop it and start a bolus of 20% lipid emulsion. 09:05 I don't know how it works but it works. 09:13 Is it? I haven't used it, so I'm not sure. 09:27 Is lipid emulsion tpn? I don't know. 09:31 Okay, that's right, yeah. 09:34 Anyway, so TPN, XML change it to TPN. 09:37 Okay. 09:37 Okay, so that's you need to remember lipid emulsion. 09:41 That's it. 09:41 So local anesthetic as I said, safe dose is probably the most important thing you need to remember.
About the Lecture
The lecture Local Anesthesia by Stuart Enoch, PhD is from the course Trauma and Post-OP Management.
Included Quiz Questions
What is the first step in assessing a trauma patient after an acute injury?
- Assessing the airway
- Assessing breathing
- Assessing circulation
- Assessing for a head injury
A 5-year-old child is seen sitting in a tripod position, drooling and with the head hyper-extended. On auscultation, inspiratory stridor is heard. Which of the following is contraindicated in this child?
- Oral Intubation
- Flexible fiberoptic laryngoscopy in the OR
- Tracheostomy
- IV Antibiotics
An 18-year-old female presents to the ER after being crushed in a boating accident. She has open wounds all over her anterior legs. The posterior legs are edematous without bruising, and has shiny, tight, firm skin that is extremely tender. Pedal pulses are diminished bilaterally. Which is the best next step in the management of this patient?
- Fasciotomy
- Compression with ice
- Analgesics
- Rest
A 6-year-old child was playing at the park at noon, while feeding the animals, he was suddenly bit by a raccoon. What is the most important question that the doctor should ask?
- Tetanus status of the child
- How old is the child?
- Which park was he in?
- How did the raccoon look?
A 5-year-old child was playing baseball when suddenly another player’s bat hit his arm. Imaging shows a 12cm open fracture with severe comminution and segmental fractures. The child complains of numbness and tingling with profuse bleeding. The doctor determines that a complete flap coverage is needed. Which stage best describes the above open fracture?
- Stage III C
- Stage I
- Stage II
- Stage III A
How are open wounds described according to the Gustilo classification of Stage II open fractures?
- Greater than 1 cm
- Less than 1 cm
- Greater than 10cm
- Greater than 0.5cm
A 13-year-old soccer player suddenly twisted his ankle while playing. Upon examination he was found to have reduced blood flow to he ankle area with intense pain. Which of the following best describes his diagnosis?
- Compartment syndrome
- Ankle sprain
- Comprimised syndrome
- Spinal cord laceration
An ER patient was diagnosed with compartment syndrome. His vitals were 160/102 mm Hg. The surgeon decides to decompress the patient’s affected leg. The patient’s differential pressure should not exceed?
- 30 mmHG
- 35 mmHG
- 40 mmHG
- 50 mmHG
An 18-year-old female was hit by a robber on the head. In the ER a medical student decides to assess the patient. She withdraws and opens her eyes to painful stimuli. Her speech is incomprehensible. Which of the following best describes her Glasgow coma scale score?
- 8
- 9
- 10
- 12
A 65-year-old alcoholic was found to be obtunded and unconscious on the floor on a cold winter’s night by a local pub. The patient had several vodkas, no food and decided to take a double dose of his daily medication that he normally takes while eating. What would be the most likely finding on his blood test results?
- Hypoglycemia
- Hyperglycemia
- Hypocalcemia
- Hypercalcermia
A 21-year-old male was found at a local disco on the floor. He was unconscious, had difficulty breathing and was observed to have tiny pupils. The patient was rushed to the ER and was given medication to reverse his symptoms, upon which he became irate. What is the possible cause of this patient's condition?
- Overdose on codeine
- Overdose on alcohol
- Overdose on marjuana
- Overdose on tobacco
Which of the following is not an indication for a CT scan after a traumatic brain injury?
- Amnesia for events >15 minutes before impact
- GCS <13 on initial assesment in ER
- Post-traumatic sezuire
- Basal skulll fracture
What does The Monro-Kellie doctrine state?
- The cranial compartment volume is incompressible and the cranium volume is fixed
- An increase in volume in one of the cranial areas must be compensated by increase in the volume of the other
- The cranial compartment volume is compressible and the cranium volume is fixed
- The cranium’s constituents creates volume disequilibrium
What happens to peripheral pressure during cerebral edema?
- Decrease
- Increase
- Stay the same
- Is of no concern
A hospitalized patient had his vitals taken early in the morning after blood loss from trauma. 1800 ml of blood was lost. The patient is currently tachycardic and tacypneic with a pulse of 131, and a blood pressure of 88/51 mm Hg. Which of the following best describes the patient's current state?
- Class III shock
- Class V shock
- Class II shock
- Class IV shock
An unresponsive child was found after being struck by a moving bus. It was estimated that he had lost 700 ml of blood. The patient’s vitals are as follows, pulse 88, blood pressure of 101/70 and RR 18. Which of the following best describes the patient's current state?
- Class I shock
- Class II shock
- Class III shock
- Class IV shock
A volleyball player fell and and landed on her outstretched hand. Two weeks later, she complained of pain on the radial and dorsal aspect of the hand. What would be the most likely diagnosis after imaging the patients hand?
- Scaphoid fracture
- Ulnar nerve compression
- Humerus fracture
- Radial artery embolsim
A patient suffered a hand injury after falling foward in which he used his palm to catch himself on the floor. The patient was found to fracture a bone in the radial most side of his hand. Which is the next best intial step in investigating the injury?
- Plain x-ray
- MRI
- Ct scan
- Ultrasound
Which of the following is the best form of imaging to identify hip fractures?
- AP and lateral views of the hip
- Lateral views of the hip
- Vertical views of the hip
- Oblique views of the hip
An 80-year-old female was found on her bathroom floor unable to ambulate. Imaging shows a fracture of her hip. What specific finding would be found on imaging of her affected leg?
- Shorterned externally rotated leg
- Lengethened externally rotated leg
- Shorterned internally rotated leg
- Lengethened internally rotated leg
A 75-year-old male comes into the office complaining of intense hip pain after falling in the snow, IImaging shows a hip fracture affecting the capsule. Management decided to be either conservative or internal fixation. What type of fracture does the patient have?
- Undisplaced intracapsular hip fracture
- Displaced intracapsular hip fracture
- Undisplaced extracapsular hip fracture
- Displaced extracapsular hip fracture
A 90 year old female is being treated in the OR for a stable extracapsular fracture. The orthopedic surgeon decides to perform a 2-part intertrochanteric procedure. Which of the following devices is most likely to be used?
- Dynamic Hip Screw
- Intramedullary nail
- Cast and recovery
- Hip replacement
A 26-year-old female was trapped in an apartment fire and suffered several burns to the face. What should be the first step in management?
- Securing the airway
- Applying lubricant
- Cooling off the patient
- Fluid resuscitation
A 12-year-old child was playing with the stove when a pot full of water fell on them. The child complained of pain and red and mottled burns, along with a few blisters were noted. Which of the following denotes the degree of the burns?
- Second degree
- First degree
- Third degree
- Fourth degree
A 46-year-old burn victim was hospitalized for fever, infection and exacerbation of his cystic fibrosis. Lab tests performed showed gram negative bacteria which secreted a blue-green pigment. The patient was then started on antibiotics. Which of the following organisms is most likely responsible?
- Pseudomonas aeruginosa
- Staphylococcus aureus
- Streptococcus pyogenes
- Streptococcus pneumoniae
Which of the following is a more accurate way of identifying pediatric burns?
- Lund and Browder
- Wallace
- Rule of 10’s
- Rule of 9’s
A 35-year-old female comes in for management of her solitary thyroid nodule. It is palpable and the doctor is concerned about malignancy. TSH levels are normal. Ultrasound shows an abnormality that is 1.5 cm. Which is the next best step in management?
- Fine needle aspiration
- Ultrasound
- Biopsy
- MRI
A 46-year-old female is diagnosed with suspected gastric cancer and arrives to your office to discuss biopsy options. She is on anticoagulants and prefers the least invasive methods. The doctor explains the pros and cons including the possibility of missing the malignancy with that option. Which of the following biopsies is the best choice to avoid major surgery?
- Endoscopic biopsy
- Frozen section biopsy
- Incisional biopsy
- Excisional biopsy
A 19-year-old female comes in due to her concern about a black spot on her face. It has unclear margins and seems to be growing. Biopsy shows squamous cell cancer. To treat this lesion with the most efficacy based on location, which one of these procedures is best fitting?
- Mohs surgery
- Punch biopsy
- Fine needle aspiration
- Core needle biopsy
A 29-year-old female with a known sexual history presents with pubic pain and abnormal vaginal discharge. Which of the following is the best next step to further assess the patient?
- Brush Cytology
- Cervical biopsy
- Colposcopy
- Core biopsy
A 13-year-old boy comes in after a car accident with lacerations on his arms, hands, legs and abdomen. The resident on call decides to suture the fingers of the patient first. Which of the following medications should be avoided?
- Lidocaine with epinephrine
- Lidocaine
- Icing
- Mepivacaine
What is the mechanism of action of lidocaine?
- Prevents the influx of Na+ by blocking the Na+ channel within a nerve preventing propagation of the action potential
- Allows the influx of Na+ by blocking the Na+ channel within a nerve preventing propagation of the action potential
- Prevents the influx of K by blocking the K channel within a nerve preventing propagation of the action potential
- Prevents the influx of Na+ by blocking the Na+ channel within a nerve, allowing propagation of the action potential
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |