Playlist
Show Playlist
Hide Playlist
Large Airways Obstruction: Investigation and Treatment
-
Slides 05 MajorAirwaysObstructionBronchiectasis RespiratoryAdvanced.pdf
-
Download Lecture Overview
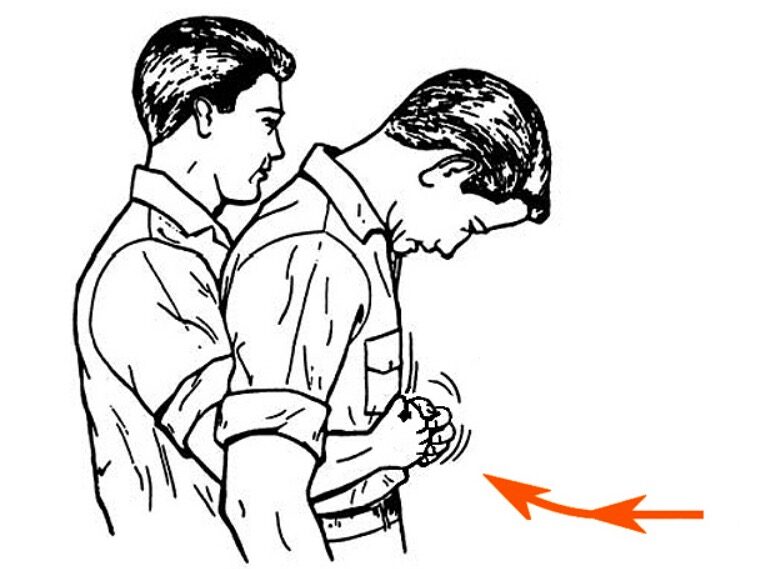
00:00 So what are the clues that somebody has an obstruction of the trachea or a major bronchi? Well they'll have obstructive spirometry and a low peak flow, but unlike asthma, it won’t vary. It's not a reversible cause of airways obstruction. The symptoms tend to be positional, so the patient may lie down and feel worse, or sit back up again and feel better, whereas in asthma it would be diurnal. The patient is worse at night, coughs in the morning, but is better in the evening. In large areas obstruction, the wheeze is usually inspiratory. Stridor rather than inspiratory which is the wheeze that you might get with asthma or COPD. There may be a history that explains the potential cause for large airways obstruction or a history of prolonged intubation for whatever reason in the past suggesting there may be a tracheal stenosis. The flow volume loop is very helpful, because that can show a very characteristic change that you get with large airways obstruction with flattening of the inspiratory and expiratory flow volume loops, and that's shown in this diagram on the right hand side of the slide. But obviously you need to do a flow volume loop to see this appearance, and most patients presenting with cough and airways obstruction may not get a flow volume loop. So again, that comes back to the high index of suspicion. 01:20 If somebody may have large airways obstruction, do a flow volume loop. Another clue is that the peak flow falls in a greater way relative than the FEV1, and that's because the peak flow is largely dependent on flow down the larger airways, whereas FEV1 is largely dependent on flow down the smaller airways. So the peak flow will be very low, and the FEV1 may be quite low but not nearly as low as you might expect for how low the peak flow is. How do you investigate these patients? Well, peak flow, lung function tests, flow volume loop as already discussed. X rays of the chest to the neck can show changes as the mediastinal tumor, there may be mediastinal mass invisible for example. But the important investigation is the CT scan, that's the definitive X ray and that should show where there's a mass obstructing the larger airways and you can see an example here of a CT scan where somebody with a very large mediastinal tumor, that's the sort of heterogeneous grey mass in the middle of the x-ray and the trachea has a very small slit like object pointed to by number 1. And you can see that there's both displaced and very narrow compared to its normal position. 02:31 And if somebody has that sort of appearance or you suspect they have large airways obstruction, then the test you need is a bronchoscopy, because you can visually see the obstruction, and then you can also do biopsies to identify the cause of that obstruction although you have to bear in mind that that can be dangerous because the patient may bleed, and the extra blood on top of the obstruction may precipitate an acute large airways obstruction. And bronchoscopy can be used for treatment, as we will discuss in the next slide or two. So, somebody presenting with acute large airways obstruction that is a medical emergency. Obstructing the trachea can kill you very easily. So sit the patient up, they feel better when they are sitting up. Give them high flow oxygen, and sometimes we give them what we call heliox, and that's a 50/50 mixture of oxygen and helium and that causes the viscosity of the inhaled gas to be lower and that can get past obstruction more easily than normal air. We give patients high dose intravenous corticosteroids as a stat dose and follow that by continued intravenous doses or oral prednisolone depending on how unwell the patient is, and we do that because there may be surrounding oedema of the cause of obstruction. 03:51 So if you have tumor, as it grows it causes oedema around the surrounding tissue and that oedema can be reduced by steroids, and that makes a substantial difference to the actual obstruction to the airway. So the high dose steroids are very useful. We used nebulized bronchodilators, salbutamol and in fact we use adrenaline as well. Intravenous fluid replacement is necessary, these patients are often breathing fast and are dehydrated as a consequence. And these patients do need to be considered for free potential lifesaving interventions. One, they may need intubation. Now clearly, putting an ET tube (endotracheal tube) down somebody with a tracheal obstruction is difficult and requires specific skills because there will be a tight trachea and that will require a small tube to get past that. A tracheostomy is very beneficial as long as the obstruction is above the tracheostomy site, so that would be the high trachea or the larynx. And then patients may need bronchscopic intervention. That is not a treatment for very acute obstruction but if people are presenting with semi-acute and you have the time to arrange a bronchscopic intervention, then that may be very beneficial. Chronic treatment. So somebody has an airway obstruction, it's been identified by peak flow and flow volume loop and a bronchoscopy, how do you get past that obstruction, how do you sort it out? Well, it depends on the cause. Somebody has a cancer, then you would use radiotherapy, potentially to improve that. There is also a variety of bronchoscopic interventions that can be used to get past large airways obstruction and these include laser ablation over tumors eroding into the trachea for example, or you could put stents across tight areas, which will open up and push the stenosis away. And then, surgery could be considered. That could remove the cause of the tumor for example, especially the benign tumors of the trachea. And then tracheostomy could be a long term way of avoiding chronic obstruction, but again that has to be a high airways obstruction somewhere up in the upper trachea or the larynx.
About the Lecture
The lecture Large Airways Obstruction: Investigation and Treatment by Jeremy Brown, PhD, MRCP(UK), MBBS is from the course Airway Diseases.
Included Quiz Questions
Which of the following would suggest asthma rather than large airway obstruction?
- Significant diurnal variation and symptom reversibility
- Very limited improvement in low peak flow recordings with treatment
- Positional symptoms
- Flattening of the inspiratory and expiratory flow-volume curves
- Stridor
A 2-year-old boy is brought to the emergency department with dyspnea and drooling. He has had a fever for 2 days. His past medical history is unremarkable. He is in a tripod position and appears agitated. Physical examination shows stridor. Which of the following is the most appropriate next step in management?
- Orotracheal intubation
- Antibiotics
- Cricothyrotomy
- Chest X-ray
Which of the following is NOT an appropriate immediate management step for a patient presenting with signs of acute severe obstruction of the upper airways?
- Spirometry
- Sitting the patient up
- Intravenous high-dose corticosteroids
- High-flow oxygen
- Endotracheal intubation
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |