Playlist
Show Playlist
Hide Playlist
Ischemic Heart Disease: Clinical Manifestations and Pathophysiology
-
Slides Ischemic Heart Disease.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
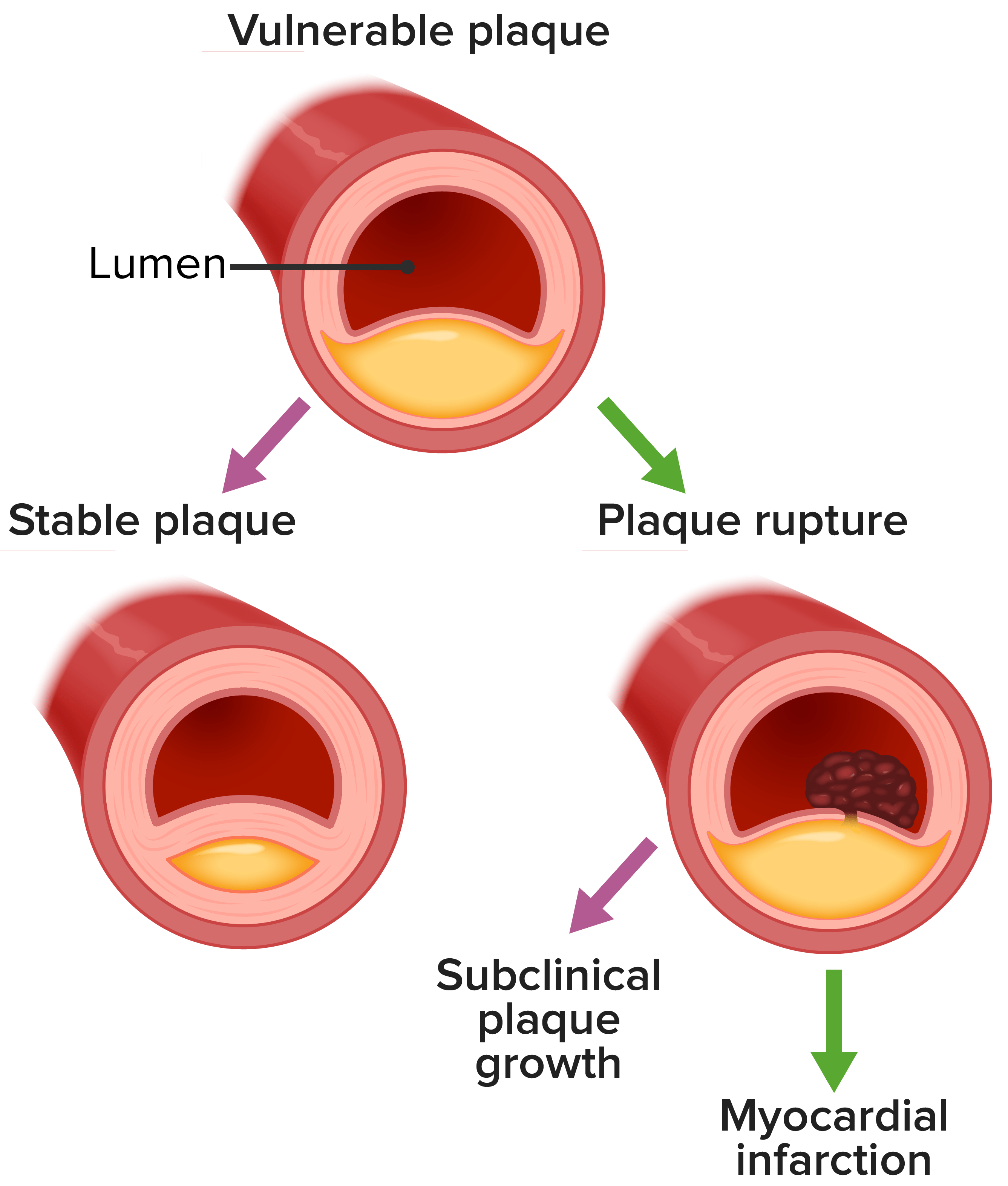
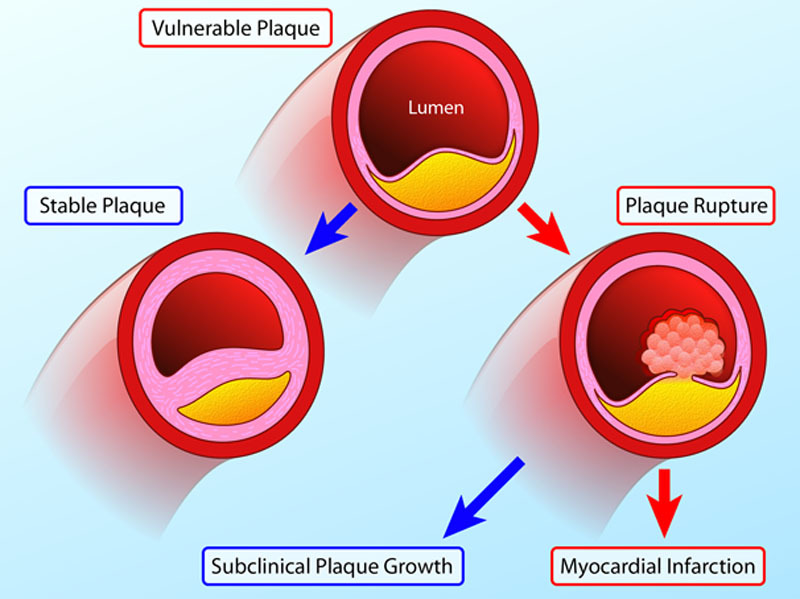
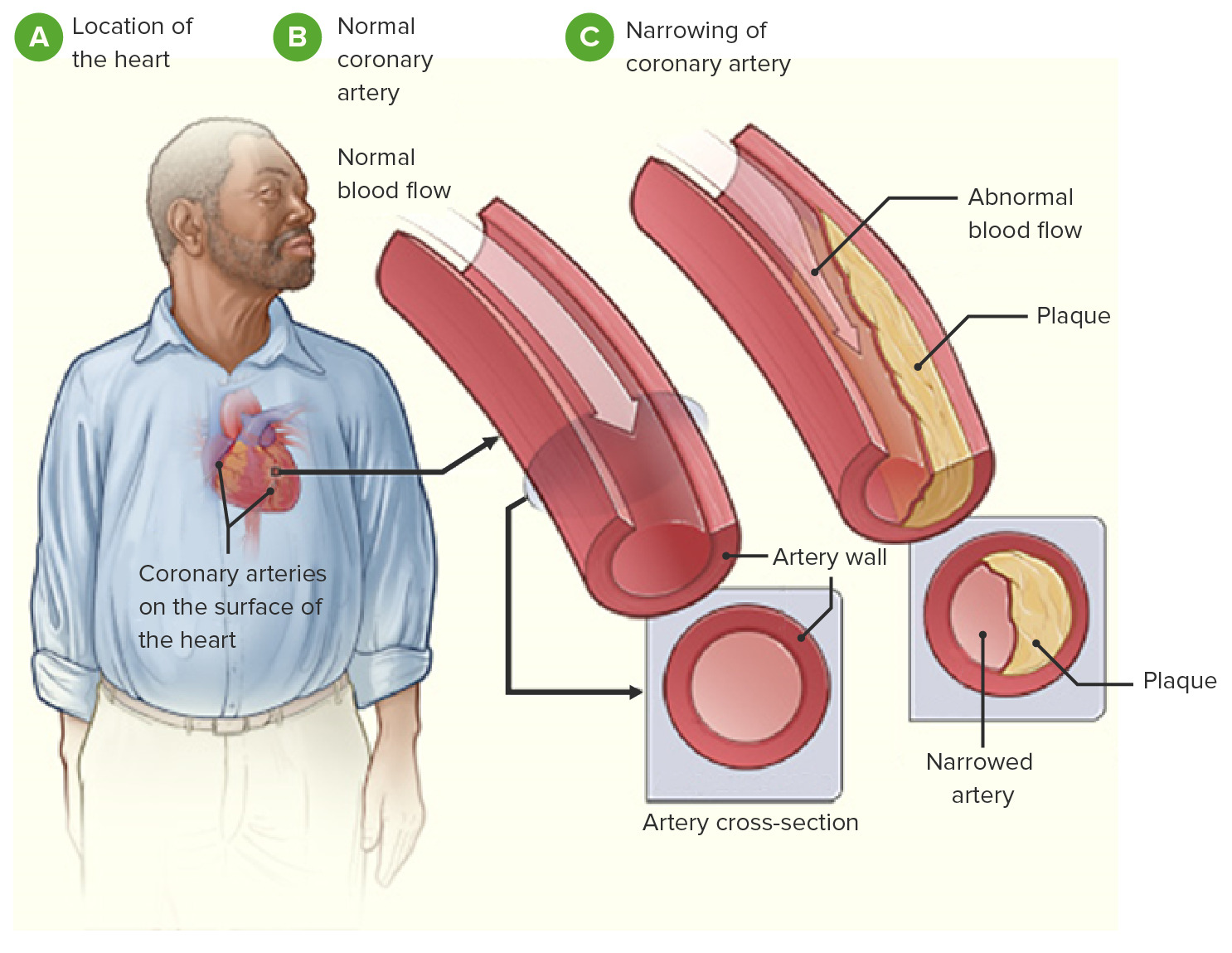
00:00 So other symptoms of ischemic heart disease, and basically, this has to do with a dysfunctional heart. 00:08 So if the heart is not squeezing appropriately. 00:10 It's got systolic dysfunction because of ischemia, you're going to have low flow and you will have symptoms of dyspnea. 00:14 you're going to have low flow and you will have symptoms of dyspnea. 00:17 So you will be short of breath. 00:19 You may have abnormal conduction through the heart. 00:22 That will give rise to palpitations. 00:24 You may have inadequate perfusion of the rest of the vasculature. 00:29 So you get dizziness. You can even have syncope. 00:33 There is a sense of restlessness and anxiety. 00:35 A feeling of doom and gloom, particularly, if you're having an acute myocardial infarct. 00:40 This is probably due to activation of a neurohumoral axis, but you actually feel like, "I'm going to die." Sometimes, you're right. 00:50 And then you can have other autonomic symptoms. 00:53 So diaphoresis, sweating, nausea and vomiting. 00:56 Those are typically associated with posterior wall ischemia, so that we are activating the vagal nerve. You can also have syncope. 01:04 If you activate the vagal nerve enough, you can go into bradycardia. 01:07 Alright. So some other interesting pathophysiology of atherosclerotic ischemic heart disease. 01:14 So this is just showing you a progression over years of an atherosclerotic plaque. 01:20 On the left-hand side is a normal coronary artery with a nice normal media and no intimal hyperplasia. 01:28 And you can grow that atherosclerotic plaque for a long time. 01:31 Up to that point shown there on the fourth circle where the luminal diameter hasn't changed. 01:40 It's the same blood flow through that vessel, even though I got more and more and more atherosclerotic plaque. 01:46 That's because there's outward remodeling of the vessel. 01:50 So even though I'm getting a thicker intima and the wall is getting thicker locally, the vessel is dilating and adapting. That's the Glagov phenomenon. 01:59 Now, there's an upper limit to this adaptation, and it occurs kind of right around when you have 70% stenosis. 02:07 At that point, the atherosclerotic plaque wins, and the ability of the vessel wall to expand is inadequate to keep up. 02:14 So now, with that critical stenosis, the 70% stenosis, you could potentially start becoming symptomatic. 02:21 And actually, if the atherosclerotic plaque progresses, you can develop now, anginal symptoms, even without an infarct, even at rest. 02:30 So the last one on the right is just showing you a very small pinpoint lumen, and that may be limiting even at rest in terms of providing adequate nutrition and oxygenation to the heart muscle. 02:43 So let's think about this looking in a slightly different way. 02:48 We're going to look at the lumen of a coronary artery, and over the course of decades as indicated at the top, you can have a progressive evolution of atherosclerosis. 03:02 Atherosclerosis has a very long timeline. 03:05 It doesn't in most people occur within weeks or months. It takes years and decades. 03:12 So you can have up to six decades before it begins to be a significant occlusion. 03:18 At that 70% stenosis, that's critical. 03:21 That will give - that critical stenosis will give you stable angina. 03:25 So running around the block pretty reliably gives you chest pain. 03:29 And then you can have plaque rupture. 03:32 And within minutes, you go from whatever degree of occlusion you had, to now, a completely occluded vessel. 03:39 Manifesting as an acute coronary syndrome, unstable angina and remember that the majority of such plaque ruptures occur on vessels that are less than critically stenotic. 03:53 So that are 20%, 30%, 40%, 50% chronically stenotic, alright? With that thrombus formation and complete occlusion of a vessel, then you can have a myocardial infarct.
About the Lecture
The lecture Ischemic Heart Disease: Clinical Manifestations and Pathophysiology by Richard Mitchell, MD, PhD is from the course Ischemic Heart Disease.
Included Quiz Questions
What is the term that describes vascular remodeling to maintain constant flow despite increases in atherosclerotic lesion mass?
- Glagov phenomenon
- Raynaud phenomenon
- Uhthoff phenomenon
- Trousseau syndrome
- Coronary steal syndrome
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
1 customer review without text
1 user review without text