Playlist
Show Playlist
Hide Playlist
Introduction to Breast Imaging
-
Slides Introduction to Breast Imaging.pdf
-
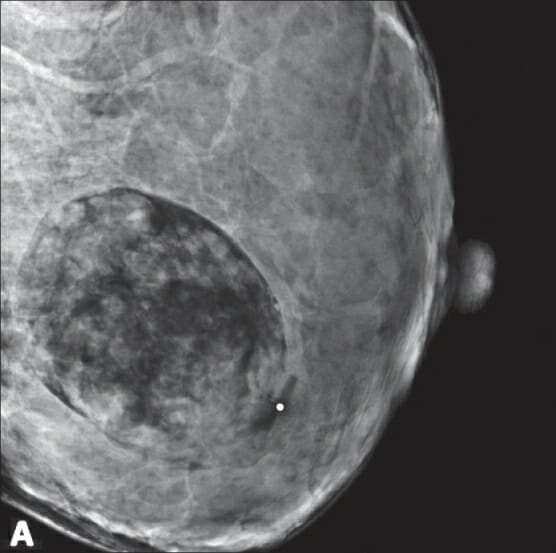
Download Lecture Overview
00:01 So let's move on to the breast imaging portion of our radiology course. 00:04 In this lecture we'll go over breast cancer in general and an overview of what mammography is. 00:10 So breast cancer is the most common cancer in women worldwide. 00:13 Early detection and treatment has been proven to save lives and the only proven method for breast cancer detection is mammography. 00:21 So mammography is a type of radiograph of the breasts. 00:26 It involves two views of each breast to ensure that all of the breast tissue is included. 00:30 It's important to remember for patients that are afraid of the radiation involved in the mammography that the amount of radiation that the patient receives in a standard mammogram which is four views, two on each side, is the same amount of radiation that they would receive in about three months of exposure to their surroundings or one transatlantic flight. 00:48 Compression is always performed when doing mammography. 00:53 Compression of the breast tissue is necessary in order to spread out the tissues and visualize any abnormalities that may be hidden within them. 01:00 The compression paddle is made of very firm plastic. 01:03 The amount of compression is between about 12 and 18 kilograms of pressure and it can be very uncomfortable so it's important to remember that this is an essential part of the examination. 01:13 So this is an example of a normal screening mammogram. 01:17 We have two views on the right and they're called the MLO and the CC view and then we have two views on the left which is called the MLO and the CC view. 01:26 We'll go over some of the anatomy in just a minute. 01:29 So screening mammograms are performed on patients with no clinical breast symptoms. 01:33 Again, we have four total images and MLO stands for Medial-Lateral-Oblique. 01:38 So this images performed almost as a lateral but it's oblique a little bit in order to get the upper outer part of the breast into the film. 01:46 This part of the breast is important because it often contains the most glandular tissue and most of the breast cancers may occur in this region because of that. 01:53 The CC views stands for cranial caudal so in this view the breast is compressed horizontally and you can see that the top part of the CC view is actually by convention the lateral aspect of the breast and the bottom part of the CC view is by convention the medial aspect of the breast. 02:10 On the MLO's it's as if you would expect up here would be the superior part of the breast. 02:16 Down here is the inframammary fold or the inferior part of the breast and then here, the whiter area is the pectoralis muscles seen posteriorly. 02:25 So ideally, women should be screened every year beginning at the age of 40 and this should continue as long as they have a life expectancy of about 10 years or more. 02:34 There have been about 7 worldwide large randomized controlled trials that have shown about a 30% decrease in deaths from breast cancer due to screening mammography. 02:43 However, mammography done annually can be expensive and for this reason it's not done in many parts of the world. 02:49 so what is a diagnostic mammogram? Mammograms are divided into screening mammograms which is performed on a patient that doesn't have any symptoms or a diagnostic mammogram and this is performed on a woman that usually has a presenting symptom. 03:03 So either she has clinical evidence of breast disease, she's presenting with the palpable mass or other symptom, or she's coming back because we see an abnormality on a screening mammogram. 03:13 So screening mammograms are usually read after the patient leaves. 03:17 They're performed in bulk and the radiologist looks at a whole bunch of them at the same time so women who have an abnormality on a screening mammogram are usually gone by the time the mammogram is read. 03:26 They then come back if there's an abnormality that's visualized. 03:29 On a diagnostic mammogram, we perform additional tailored images that further evaluate the area of concern. 03:36 So abnormalities that lead to a diagnostic study include a palpable mass, pain, nipple discharge, skin thickening, skin or nipple retraction, or again any kind of abnormality seen on a screening mammogram so these can all be signs of breast cancer. 03:55 What is breast density? So the breast tissues are made up of fibroglandular tissue and fatty tissue. 04:03 The density of the breast is based on the amount of fibroglandular tissue that's present and on a mammogram fibroglandular tissue appears white. 04:11 So there are four major tissue densities: almost entirely fatty, scattered fibroglandular which both represent non-dense breast tissue, then there are two categories of dense breast tissue: one is heterogeneously dense and then one is extremely dense and so this ranges on the spectrum of very fatty all the way to very dense. 04:32 Dense breast tissues actually decrease the sensitivity of mammography and they're thought to have at least a slightly increased risk of developing breast cancer. 04:42 We don't know exactly how high that risk is and there's researches currently being done on that to see how high that risk is. 04:49 So this is an example of a patient with almost entirely fatty breast tissues. 04:56 S you can see that the fat here is the area that's black or dark gray and that encompasses the majority of the breast. 05:04 The fibroglandular tissues are the white areas so there's very little fibroglandular tissue in this patient. 05:10 This is an example of scattered fibroglandular tissue and you can see that there's more white now that's interspersed within the fatty areas. 05:18 This is an example of a heterogeneously dense breast and there's a lot more white now than there is dark. 05:26 So you can see that there is much more fibroglandular tissue in this patient. 05:29 And then lastly, this is an example of extremely dense breast tissue. 05:33 So this patient has very white breasts as seen on the mammogram and this can actually hide cancers because cancers can also appear white. 05:42 So this is why the sensitivity of a patient with extremely dense breast tissue is decreased on mammography. 05:48 So what kind of tissue pattern is this? You can see very dark areas through the breasts and then you can see a very large pectoralis muscle here which you can see very well on the CC view as well. 06:13 So this is actually a male tissue pattern. 06:16 They usually present with large pectoralis muscle and minimal fibroglandular tissue. 06:21 Tomosynthesis is 3D mammography. 06:26 It's now used in addition to standard or 2D mammography and it's shown to increase the sensitivity of mammography especially in women with dense breast tissues. 06:35 It's a very expensive upgrade to a standard mammography machine and worldwide this is now slowly coming more into use. 06:41 So let's review some birads categories. 06:45 Every mammography report has a birads category that's assigned to it and this is a final assessment category so it tells you what should be done next if anything. 06:55 This is mandatorily assigned to every mammography report and this is again a worldwide standard. 07:00 So there are 7 major birads categories. 07:04 Birads zero means that we need additional imaging or prior mammogram for comparison. 07:10 So, we basically can't give an answer right now. 07:12 Birads 1 is completely negative. 07:15 Birads 2 is benign, so we see an abnormality that's normal to see within the breast and no further follow up is indicated. 07:23 Birads 3 means that the area that we see is probably benign so there's a less than 2% chance of malignancy. 07:30 Usually, the abnormalities that are probably benign we recommend a short term follow up. 07:35 So the short term follow up is often performed in about six months and we continue to follow this abnormality for a period of about two years. 07:42 Two years in mammography is considered the point of which something can be called benign and no further follow up will be indicated. 07:48 A birads 4 is the suspicious abnormality so there's anywhere between a 2% and 95% chance of malignancy. 07:56 In patients that have a birads 4 abnormality, biopsy should be considered and is most often performed. 08:02 Birads 5 means that the abnormality is highly suggestive of malignancy so there's a greater than 95% chance of malignancy. 08:10 In this case, a biopsy is always performed for further evaluation. 08:15 And then birads 6 is the known biopsy proven malignancy that's currently within the breast. 08:20 So a patient that's been treated for breast cancer is not given a birads 6. 08:25 This is a patient that has a recently biopsied proven malignancy that has not yet been treated. 08:31 So I have given you a general overview of the field of breast imaging. 08:35 We've gone over the birads categories which are very important for everyone to know because it tells you what kind of follow up is indicated in this patient. 08:41 So let's now move on to discussing some abnormalities within the breast.
About the Lecture
The lecture Introduction to Breast Imaging by Hetal Verma, MD is from the course Thoracic Radiology. It contains the following chapters:
- Mammography
- Breast Density
Included Quiz Questions
Which description matches BI-RADS categories number CORRECTLY?
- BI-RADS 4 indicates a 2-95% chance of malignancy.
- BI-RADS 3, a biopsy should be considered.
- BI-RADS 2 requires a follow-up in 6 months.
- BI-RADS 5 indicates a 2-95% chance of malignancy.
- BI-RADS 0 indicates a biopsy-proven carcinoma.
Which statement regarding mammography is FALSE?
- A screening mammogram is performed in patients with either tenderness or self-felt mass.
- A total of 4 images, two on each side, are taken, MLO and CC.
- It is the only proven method for breast cancer screening.
- Compression of the breast tissue is necessary to spread out the breast tissues and visualize abnormalities.
- Ideally, women should be screened every year, beginning at the age of 40 and continuing as long as they have a life expectancy of more than 10 years.
Which of the following is not a type of breast density?
- Localized fibroglandular
- Almost entirely fatty
- Scattered fibroglandular
- Heterogeneously dense
- Extremely dense
Which of the following regarding tomosynthesis is TRUE?
- It is slowly coming into use worldwide.
- It increases the sensitivity of mammography, especially in women with fatty breast tissue.
- It is a combination of 3D and 2D mammography.
- It is used instead of routing 2D mammography.
- It is a very cheap upgrade to the standard mammography machine.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |