Playlist
Show Playlist
Hide Playlist
Insulinoma
-
Slides Insulinoma Surgery.pdf
-
Download Lecture Overview
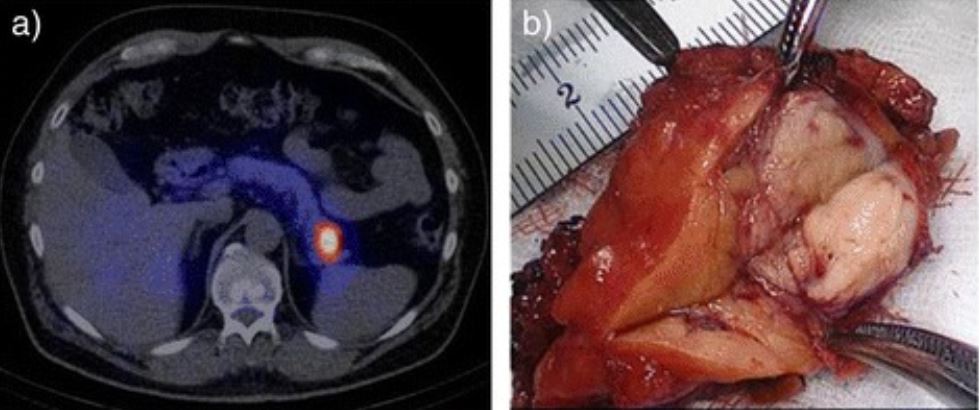
00:00 Welcome back. Thanks for joining me on this discussion of insulinomas under the section of general surgery. As a reminder, endocrinopathies in general, whether it’s in a section of medicine or surgery are incredibly high-yield for the USMLE examinations. Let’s start discussing insulinomas. 00:21 Insulinomas result in autogenous insulin secretion usually associated with a pancreatic islet cell tumor. 00:31 The main finding is hypoglycemia. Symptoms of hypoglycemia include sweating, dizziness, confusion, and palpitations. You’ve probably had episodes of hypoglycemia yourself and it’s an unforgettable feeling. Also remember that multiple endocrine neoplasias, all three types, are incredibly high-yield. Let’s review the multiple endocrine neoplasia type 1. They consist of parathyroid tumors, pituitary tumors, and specific to our topic right now, pancreatic tumors. 01:08 They contain gastrinomas and insulinomas. On routine laboratory values, the chemistries and the CBCs are unlikely to be very helpful. However, high serum insulin levels despite low fasting glucose is almost absolutely necessary for the diagnosis of insulinoma. Here’s a schematic of the distribution of the functional neuroendocrine tumors of pancreas. Remember that insulinomas and gastrinomas are both categorized as neuroendocrine functional tumors of the pancreas. Here’s a depiction of an upper endoscopy with an endoscopic ultrasound. 01:55 Oftentimes, this is one of the most helpful modalities to locate the actual insulinoma or neuroendocrine tumors of the pancreas in general. This procedure is performed by doing a routine EGD with a special probe that contains an ultrasound probe at the end of the tip. 02:17 Here’s a cross-sectional imaging, a CT abdomen/pelvis demonstrating insulinoma. Note on the image that the insulinoma is in the mid body of the pancreas. At surgery, this is a high definition laparoscopic view. Notice on the image here that the fat pad in the middle of the screen depicts the fat overlying the pancreas. As you can see, the pancreas is exposed and the insulinoma can be enucleated. I’d like to pose a question to you. What is factitious hypoglycemia? I’ll give you a second to think about it. Factitious hypoglycemia results from exogenous insulin administration. In clinical scenario, it’s classically associated with medical professionals such as doctors or nurses. It results in hypoglycemia, hyperinsulin, but unlike actual insulinomas, the patient actually has a normal to low C-peptide level. Very important clinical pearl: factitious hypoglycemia can be differentiated based on the C-peptide levels. So, in patients with chronic hypoglycemia or symptoms of insulinoma, make sure you get an insulin level as well as a C-peptide level. 03:39 Once again, as a high-yield topic, the C-peptide is what differentiates an insulinoma versus exogenous insulin administration. Thank you very much for joining me on this discussion of insulinomas.
About the Lecture
The lecture Insulinoma by Kevin Pei, MD is from the course General Surgery.
Included Quiz Questions
Which genetic syndrome is associated with neuroendocrine tumors of the pancreas?
- MEN 1 syndrome
- MEN 2A syndrome
- MEN 2B syndrome
- BRCA 1 syndrome
- BRCA 2 syndrome
A patient presents with recurrent sweating, dizziness, confusion, and palpitations. What would you expect to find on laboratory tests that would support a diagnosis of a pancreatic islet cell tumor (an insulinoma)?
- Elevated insulin level, low fasting glucose level, elevated C-peptide level
- Low insulin level, high fasting glucose level, high C-peptide level
- Elevated insulin level, low fasting glucose level, low C-peptide level
- Elevated insulin level, elevated fasting glucose level, elevated C-peptide level
- Elevated insulin level, high fasting glucose level, low C-peptide level
A 53-year-old nurse presents with recurrent sweating, dizziness, confusion, and palpitations. On laboratory exams, her complete blood count is normal, lactate is normal, blood glucose level is low, insulin level is high, and C-peptide level is low. What is the most likely diagnosis?
- Exogenous insulin administration
- Insulinoma
- A functional pancreatic islet cell tumor
- Type 1 diabetes
- Type 2 diabetes
Which imaging modality can be used to identify an insulinoma's location in the pancreas AND obtain a biopsy?
- EGD with EUS
- Computed tomography scan
- Plain abdominal x-ray film
- PET scan
- MRI scan
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |