Playlist
Show Playlist
Hide Playlist
Insomnia
-
Slides Insomnia AcuteCare.pdf
-
Download Lecture Overview
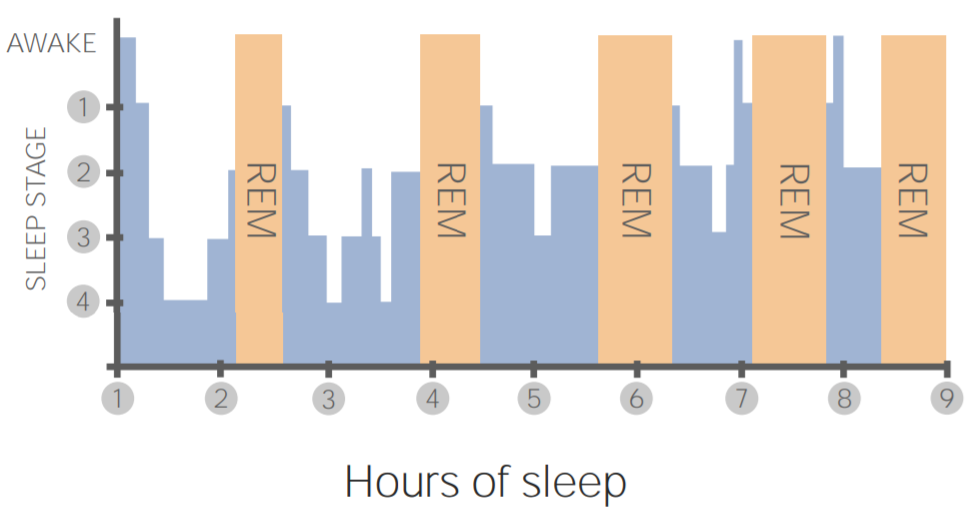
00:01 Right. 00:02 Let's all wake up and talk about insomnia. 00:04 Insomnia is a very common condition we see in primary care. 00:07 It can promote a lot of anxiety and worry in my patients. 00:11 And the funny thing is that leads to a cycle where they experience more insomnia. 00:15 So, therefore, breaking the cycle is really, really important. 00:18 So, we’ll talk about sleep and some general properties of sleep and then focus on defining insomnia and how to treat it appropriately. 00:28 So, I’m going to start with a case. 00:29 I’ve got a 50-year-old female. 00:32 She experiences early and middle insomnia and she has daytime fatigue. 00:36 That means she has trouble initiating sleep. 00:39 She has trouble with staying asleep in the middle of the night and she gets tired. 00:44 You know what fatigue is. 00:45 She gets tired in the day. 00:47 She doesn’t have any significant medical illnesses thankfully. 00:50 And a review of systems and a physical examination are negative. 00:54 So, what do you do now? Is it, A, do you recommend sleep hygiene and a sleep diary? B, initiate a laboratory evaluation? C, just start treating with something like a melatonin antagonist or agonist? Or D, initiate a 4 to 6 week trial with a hypnotic drug? Here, I would strongly argue for A because this patient, we don’t know enough about her insomnia yet. 01:21 A sleep diary can be a great way to actually document just how severe the insomnia is when it bothers her. 01:27 May give some clues too with – maybe it's stress or something related to her life, with her work, her family, where she has certain shifts where she’s staying up late. 01:36 And then working on sleep hygiene is always a good idea and highly effective. 01:42 And we’ll be talking about that quite a bit. 01:45 So, just to define insomnia, it's a subjective perception of difficulty with sleep initiation, duration, consolidation or quality that occurs despite the adequate opportunity for sleep. 01:57 So, in a situation where you're sharing a bedroom with like 14 other people and you're having a hard time sleeping, that doesn't necessarily qualify it’s insomnia because that's not really an adequate opportunity. 02:13 If you’re sleeping on a factory floor, that's not an adequate opportunity. 02:17 And it also needs to involve some form of daytime impairment. 02:22 Acute insomnia is considered less than three months in duration and chronic is longer than that, longer than three months. 02:30 So, in terms of epidemiology, it's very common. 02:34 Insomnia affects 10 to 30% of adults. 02:37 It’s more common in women. 02:38 It’s more common as you get older. 02:41 It’s definitely more common in chronic pain. 02:43 Chronic pain and insomnia tend to go hand-in-hand. 02:46 And unfortunately, they exacerbate each other. 02:48 So, patients who sleep less also have more pain. 02:53 And it can be hereditary. 02:54 It tends to run in families, insomnia. 03:00 And it is also associated with – besides feeling tired during the day, it is associated with some more severe consequences, such as cognitive difficulty. 03:08 It’s also associated with a higher risk of accidents. 03:12 And it’s also associated with a higher risk of mood disorders as well. 03:15 So, insomnia can be a feature of anxiety and depression, but it can also promote worse anxiety and depression. 03:24 And finally, chronic insomnia is linked to intravascular inflammation and a higher risk for cardiovascular disease. 03:33 Now, sleep does change with age and I think it's important to counsel older adults because many of them are less satisfied with their sleep overall. 03:41 So, it's good to think about how sleep naturally changes with age. 03:45 There's more of a latency. 03:46 So, patients may complain of early insomnia symptoms. 03:49 It takes longer to get to sleep. 03:51 They also have reduced time in REM as you get older and they are more likely to wake up. 03:57 That said, it's a fallacy that sleep always – duration always decreases as you get older. 04:04 It can. 04:05 It can also stay about the same. 04:08 But generally, as I said, patients who are older have less satisfaction with their sleep. 04:13 And it’s due to all of those causes. 04:14 It takes longer to fall asleep. 04:16 Plus, they are waking up more in the middle of the night. 04:18 And so, therefore, it's something to counsel patients about and tell them this is going to be a normal part of aging. 04:24 Just that reassurance is a good start as a therapeutic relationship.
About the Lecture
The lecture Insomnia by Charles Vega, MD is from the course Acute Care.
Included Quiz Questions
Which of the following patients has chronic insomnia?
- A 36-year-old woman having difficulty falling asleep resulting in daytime dysfunction for 4 months
- A 24-year-old woman having difficulty maintaining sleep resulting in daytime dysfunction for 20 days
- A 78-year-old man who has daytime dysfunction as a result of waking up too early for 3 weeks
- A 16-year-old man who has slept late at night over the past year but functions well at school
- A 43-year-old woman who always wakes up early for work on weekdays despite sleeping late most nights
Which of the following is NOT associated with chronic insomnia?
- Inflammatory bowel disease
- An increased risk of cardiovascular disease
- An increased risk of developing mood disorders
- Chronic pain
- A family history of insomnia
Which of the following are natural sleep changes that occur with aging? (Choose all that apply.)
- More frequent night time awakenings
- Decrease in sleep latency
- Increase in rapid eye movement sleep
- Increase in restful sleep
- Slightly reduced or same total sleep time
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |