Playlist
Show Playlist
Hide Playlist
Infection-associated Glomerulonephritis – Nephritic Syndrome
-
Slides Nephritic Syndrome.pdf
-
Reference List Nephrology.pdf
-
Download Lecture Overview
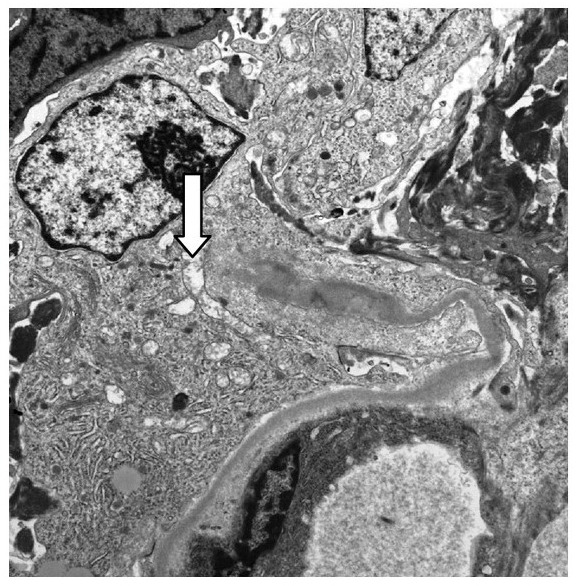
00:01 So, post-infectious glomerulonephritis, also termed infection-associated glomerulonephritis, is the most common cause of acute nephritic syndrome. 00:10 It's more common in developed countries and it has a peak incidence that's actually bimodal. 00:15 We can see it in children ages 5-12 years but we also see it again appearing in our adult population, particularly over the age of 60. 00:24 When we think about the etiology, post-infection or infection-associated GN develops in response to an infection. 00:31 So, classically, it's described as an acute nephritis that temporally correlates with an infection. 00:37 So, typically occurring 1-6 weeks following an infective illness. 00:43 And again, in the traditional sense, post-infectious really was used to describe an infection-related GN in response to streptococcal pharyngitis or impetigo, a skin infection which is also caused by strep. 00:59 Now, it's important to note that it may also occur secondary to other bacterial or viral illnesses. 01:05 These are things like staphylococcal endocarditis, pneumonococcal pneumonia, and meningococcus, viruses like hepatitis B, C, HIV, or EBV, and then parasitic infections like malaria and toxoplasmosis. 01:21 And I can say in my clinical practice where I see infection-related glomerulonephritis, probably most often happens in my patients who are infected with staph. 01:31 So, when we think about the pathogenesis of infection-related or post-infectious GN, it is an immune complex disease that's caused by specific nephritogenic strains of bacteria or viruses. 01:46 It's best characterized in Group A beta-hemolytic Streptococcus. 01:52 Those patients will have elevated titers of antibodies to streptococcal antigens that are found in -- again, found in most patients with post-streptococcal glomerulonephritis. 02:02 That includes things like ASO, the antistreptolysin antibody. 02:06 So, that's something that we wanna pay attention and look for. 02:08 The immune complex deposition formation in patients who have infection-associated GN is going to activate complement but it does so through the alternative pathway of complement activation, hence the low C3. 02:20 Now, there's 2 different hypotheses as to the pathogenesis. 02:24 One, that their circulating immune complexes comprise of that strep antigen and recognition of an antibody. 02:31 They circulate as an immune complex and deposit within the glomeruli, activating complement resulting in injury, or the infection itself can cause alterations in intrinsic proteins that are already within the glumerular basement membrane. 02:47 They now become antigenic and then patients will make antibodies that bind to those epitopes and to those alter -- or those altered antigens, rather, and then activate complement through immune complex formation. 03:00 So, in terms of how patients clinically present, it's really variable. 03:04 You can see a whole host or a whole range of different things. 03:07 Sometimes people will be completely asymptomatic with microscopic hematuria, others will have full-blown nephritic syndrome with the most profound active sediment and become very sick very quickly. 03:20 So, how do we diagnose our patients who have infection-related or post-infectious GN? These are patients that really have probably some of the most exciting urine sediment. 03:30 It is going to be active, meaning that they're gonna have these dysmorphic red blood cells packed within that urine sediment. 03:36 So, we're gonna see those dysmorphic features with those blobs on the membrane as shown here. 03:40 We can see red blood cell cast; we can even see white blood cell cast because this is an inflammatory and exudative type of glomerulonephritis. 03:48 So, we can actually see white blood cells due to inflammation that collect within that tubule, bind to that Tamm-Horsfall protein, and then form this beautiful cylindrical cast. 03:58 We also see alternative complement pathway of activation. So, what does that mean? We're gonna see a low C3 but we're gonna have a normal complement C4 in the serum and a low CH50 or H50. 04:11 We have elevated antibody titers to extracellular streptococcal products, if strep, of course, is the inciting etiology, and we can look at something like streptozyme test which is going to measure 5 different antibodies including the ASO or antistreptolysin antibody. 04:29 Patients often times have a clinical history and laboratory findings that suggest the diagnosis. 04:34 So, particularly in my pediatric population, if I have a child who has a classical strep pharyngitis or impetigo, and temporally, 1-6 weeks later, has onset of tea-colored urine, then a renal biopsy is not always indicated in that population because it's very clear as to what's happening. 04:53 In our adult populations, we almost always have a biopsy. 04:57 Now, pathologically, these patients who have infection-associated GN probably have some of the most exciting biopsies by light microscopy shown in this H and E over here. 05:07 You can see that that glomerulous is packed full of cells. 05:11 It is hypercellular. You've got endothelial cell proliferation. 05:14 You have neutrophils that are actually circulating in there and that's what our arrow shows. 05:19 These patients have an exudative GN. On immunofluorescence, we see C3. 05:24 That makes sense because we just talked about how the alternative pathway of complement is activated. 05:29 And then on electron microscopy, very pathognomonic, again, for post-infectious GN, is to see the subepithelial humps. 05:39 So, they're on that outer aspect of the capillary loop or basement membranes. 05:43 So, we've got glomerular basement membrane, we've got immune complex deposition or that subepithelial hump, and then that sitting right underneath the potosite. 05:52 Now, there's only one other disease that has subepithelial deposits and that was membranous so it's not too hard to kinda think about that when you see the electron microscopy. 06:01 You're gonna be thinking either this is post-infectious GN or this might be membranous nephropathy. 06:06 They present very differently and the other big difference between that is that these are humps, they are very large, and membranous, remember, they have a very small, very delicate immune complexes. 06:17 So, in terms of how our patients do, overall, if you take everybody together who has infection-associated GN or post-infectious GN, most people do very well and most patients will recover. 06:30 Certainly, in our pediatric population, as always, they do so much better than adults. 06:34 They're more resilient. About 95% of those patients are gonna recover without complications. 06:38 In adults, it can be much more insidious and many of those patients will have a slow progression to chronic glomerulonephritis. 06:46 And I can say that in my own patient population, I've transplanted about 3 people who have had infection-associated GN. 06:52 In terms of treatment, there really isn't anything that we can do other than targeting the underlying infection. 07:00 So, if they still have an infection that's ongoing, we wanna be able to treat that. 07:03 For those people who really manifest more on a post-infectious process like our strep pharyngitis example, then it's really just supportive care, meaning that we're gonna treat their hypertension, we're gonna treat their volume overload, and we're gonna ensure that those patients don't have any nephrotoxic exposures.
About the Lecture
The lecture Infection-associated Glomerulonephritis – Nephritic Syndrome by Amy Sussman, MD is from the course Nephritic Syndrome.
Included Quiz Questions
Which of the following is true regarding infection-associated glomerulonephritis?
- It has a bimodal age distribution.
- A renal biopsy is necessary for the diagnosis.
- It usually starts within 5 days of streptococcal pharyngitis or impetigo.
- It is caused by inappropriate activation of the classical complement pathway.
Which of the following statements is true regarding the morphology of PSGN?
- Electron microscopy shows hump-like subepithelial deposits.
- Immunofluorescence microscopy shows linear deposition of immunoglobulins along the GBM.
- Light microscopy shows mesangial hypocellularity.
- Immunofluorescence microscopy shows the pathognomonic "full-house" pattern of staining.
Which of the following is associated with post-streptococcal glomerulonephritis?
- Elevated ASO titers
- Elevated C3, C4, and CH50 complement levels
- Low blood pressure
- Protein-to-creatinine ratio of <0.2
What is the most appropriate initial step in the management of infection-associated glomerulonephritis?
- Supportive care
- Methylprednisolone
- Mycophenolate
- Referral to a nephrologist
- Prepare for dialysis
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |