Playlist
Show Playlist
Hide Playlist
Pediatric Inflammatory Bowel Disease (IBD): Management
-
Slides Inflammatory Bowel Disease.pdf
-
Download Lecture Overview
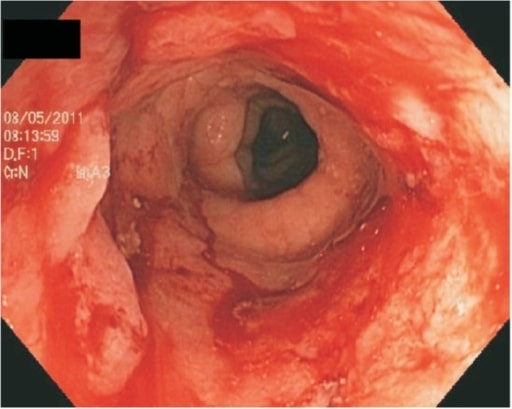
00:01 If children have Crohn's disease or ulcerative colitis, there are many treatments out there. 00:07 And it may be confusing for you at first when you're seeing your first patient to understand which treatment is due when. 00:16 This is a rapidly changing field. Just three years prior to recording this we would never have used Remicade early in disease and now we're doing that all the time. 00:27 So keep in mind that this is a changing field and lookout for changes as you go forward. 00:34 However, let's go through the major treatment options that are available to you in terms of types of treatments. 00:40 So, medications are the mainstay of management of both of these conditions. 00:44 We also have to think about nutritional considerations, how can we optimize nutrition because it is the bowel wall after all that's involved. 00:53 And also we have to think about surgical management in these patients. 00:58 So, medications. Corticosteroids, either IV or oral, it doesn't really matter are used in acute flares with moderate to severe symptoms. 01:10 These are the mainstay of therapy. 01:12 But as we know, steroid use frequently can result in all kinds of problems. 01:18 Moon faces, buffalo hump, all the findings of Cushing's disease. 01:23 We want to avoid them. 01:24 Additionally, patients may be treated by 5-amino salicylic acid. 01:30 This is usually for mild or moderate ulcerative colitis. 01:35 Patients may also get immunomodulators like azathioprine. 01:39 Azathioprine maintains remission in about 75% of patients. 01:43 Also in methotrexate is frequently used especially in patients who are failing azathioprine. 01:50 Infliximab is used both for induction and maintenance of remission. 01:56 And antibiotics such as ciprofloxacin and metronidazole are used for fistulae and pouchitis, an inflammation of the pouch left over after a surgical resection of the colon in ulcerative colitis. 02:12 Oral rifaximin improves abdominal pain and diarrhea. 02:16 Additionally, patients may receive probiotics. 02:20 This helps maintain remission and again may treat or prevent a pouchitis. 02:25 Nutritional considerations are important. 02:29 Sometimes patients require enteral feeding because they don't have the energy to keep it up. 02:34 But nutrition is so important for healing. 02:37 We often provide supplemental vitamins especially for patients with fat malabsorption where we'll give extra of the fat-soluble vitamins. 02:47 Vitamin A, D, E, and K. 02:49 Parenteral nutrition isn't uncommon especially in patients with severe small bowel disease where they have to maintain NPO status for a long period of time. 02:58 Remember, high protein levels are needed to both reconstruct your intestinal tissue and maintain your immune system's needs. 03:08 Surgical intervention is necessary in many cases. 03:13 For ulcerative colitis, colectomy with an ileal pouch and an anal anastomosis is the most optimal therapy. 03:23 And you can see here a patient who's had the green colon removed replaced by the purple small bowel. 03:30 And they've created an ileal pouch that's gonna act as sort of what was previous to the rectal vault, an area to store stool until it's time to defecate. 03:40 This patient has an ileostomy. 03:42 We can hope that this patient will have that ileostomy taken down so that he can eventually live a reasonably normal life. 03:49 In patients with Crohn's disease, fistulae and areas of stenosis can occur that can be highly problematic and periodically segmental bowel resection is needed. 04:00 These patients become very friendly with their surgeons. 04:03 They need to be followed carefully and watched for surgical issues. 04:07 The prognosis of inflammatory bowel disease is reasonably good and that these patients can live long and meaningful lives. 04:16 However, disease relapse is common. 04:19 And about more than half of patients will have a relapse within two years of their original diagnosis. 04:26 The body is constantly in an inflamed state. 04:29 So delayed puberty is common and these patients will achieve a lower final adult height. 04:35 Don't forget, especially fat soluble vitamins are a problem so these patients are at risk for vitamin D deficiency. 04:43 That and combined with their frequent steroid use put them at grave risk for bone mineral density problems. 04:51 These children can get osteopenia/osteoporosis later in life and frequent fractures. 04:57 We have to be very careful about their bone mineral density. 05:02 Some complications can occur in these patients. 05:06 Toxic megacolon can occur and that is surgical emergency. 05:11 Patients are at risk for colorectal cancer especially in ulcerative colitis. 05:17 Generally, after diagnosis for ulcerative colitis, within eight years, a patient is gonna start being screened regularly for colorectal cancer. 05:27 There is a lifelong increased risk and frequently patients will elect to have a colectomy to avoid the cancerous consequences. 05:36 Patients also have a risk for cholangiocarcinoma and generally complications of the biliary tree and -- but watching for cholangiocarcinoma is especially important in patients with inflammatory bowel disease. 05:50 So what I've tried to portray for you a picture here is that these patients can live long and productive lives. 05:57 They need help from all ailments and all sides of the medical team. 06:02 From everywhere from the medical doctors, to the surgeons, to the psychologists and to the teachers and the parents. 06:08 But together we can make their lives come out pretty well. 06:11 So, that's all I have for you about this subject today. Thanks for listening.
About the Lecture
The lecture Pediatric Inflammatory Bowel Disease (IBD): Management by Brian Alverson, MD is from the course Pediatric Gastroenterology.
Included Quiz Questions
Which is NOT a typical treatment of IBD?
- Erythromycin
- Ciprofloxacin
- Steroids
- Azathioprine
- Infliximab
Which of the following is a complication of inflammatory bowel disease that may require immediate surgery?
- Toxic megacolon
- Acute appendicitis
- Intestinal obstruction
- Acute cholecystitis
- Proctitis
Which of the following antibiotics may be employed to manage fistulae and pouchitis after surgical resection of the colon in ulcerative colitis?
- Metronidazole
- Penicillin
- Macrolides
- Isoniazid
- Rifaximin
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Excellent lecture. An important disease in pediatrics. Very clear about treatment options.