Playlist
Show Playlist
Hide Playlist
Hypertrophic Pyloric Stenosis
-
Slides GIP Hypertrophic Pyloric Stenosis.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
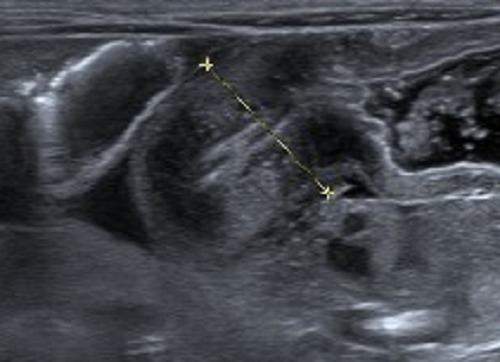
00:01 Welcome. 00:02 In this talk, we're going to cover Hypertrophic Pyloric Stenosis. 00:06 Try saying that three times quickly. 00:09 Hypertrophic Pyloric Stenosis is essentially a functional obstruction of the gastric outlet. 00:14 We're not emptying the stomach very well, and it's caused by a combination of smooth muscle hypertrophy, meaning the individual cells of the smooth muscle are bigger, but there's also more of them. 00:25 This is occurring at the pylorus for a variety of reasons that we'll get to in a moment. 00:29 This is primarily a disease of babies of neonates, and we need to recognize it in that period of time, and much less commonly an issue associated with older individuals. 00:39 We do, however, need to distinguish this from other causes of gastric outlet obstruction that could be peptic ulcer disease, cancer at that location, or a bezoar, a hairball, that literally that's what bezoar is. 00:55 So the epidemiology of the pyloric hypertrophy. 01:00 It's most common cause of intestinal obstruction in infants. 01:04 Remarkably, it occurs to some extent, in 1-3 per 1000 live births in the United States. 01:11 And that frequency pretty much holds around the world. 01:15 For reasons related to genetics, it's more common in Caucasians, whites in males, firstborns, and those who have blood groups B or O. 01:27 And clearly, if you have a family history of pyloric stenosis, there's a genetic basis for thinking that you may have it again, in another member of your family. 01:36 The etiology. 01:38 Clearly, there's a genetic basis, there's congenital disease, and it's very closely associated, for example, with trisomy 18. 01:44 Although other genetic changes may be associated with the pyloric stenosis. 01:51 It can be associated with inflammatory diseases as well, such as eosinophilic gastroenteritis. 01:59 It may be a small, but nevertheless very real side effect of drugs that are taken during gestation by mom, such as erythromycin. 02:09 Or it can be associated with defects deficits in muscle relaxation. 02:14 So if the muscle doesn't make enough nitric oxide, then you won't relax as well and you will get hypertrophy and hyperplasia of the smooth muscle. 02:24 The clinical presentation is as you expect for a gastric outlet obstruction. 02:29 So in the neonatal period of time, it usually starts within three weeks of delivery. 02:36 Initially, what will happen is that there'll be regurgitation after feeding. 02:40 So food will not be able to pass and then we'll be vomited back up. 02:46 It's typically non-bilious vomiting, because the obstruction occurs proximal to where the bile ducts dump into the duodenum. 02:56 So it's not going to be bilious vomiting, but it can be over time with very severe retrograde movement of food, it can be projectile. 03:06 The infant is clearly hungry. 03:08 The infant is not getting food delivered into the other part of the GI tract. 03:13 And so they will be anxious, irritable, they'll exhibit signs of hunger. 03:18 There won't be very good weight gain. 03:21 You may even feel with an enlarged hypertrophied muscle mass, an actual mass, a periumbilical mass where the the muscle at the pylorus is thickened. 03:34 You may also be able to perceive particularly as the infant loses weight, a gastric peristaltic wave across the abdomen after feedings. 03:42 So the stomach is trying its very best to push food through that stenosis. 03:48 And it's not able to but you'll see a very prominent gastric contraction wave. 03:54 Clearly, as the infant is not feeding appropriately, or is not able to eat and move food into the rest of the GI tract, there'll be signs of dehydration. 04:04 Diagnosis. 04:05 So it's a constellation of the clinical findings. 04:08 On the laboratories that again, it's what you might expect if there is recurrent emesis vomiting, there's going to be a hypochloremic metabolic alkalosis. 04:18 That's due to the excessive vomiting. 04:21 Because of the alkalosis, we're actually going to be chasing potassium into cells in exchange for protons. 04:28 So we'll have a functional hypokalemia. 04:32 There may be elevated blood urea nitrogen and creatinine so renal parameters are going to be elevated due to dehydration. 04:40 On ultrasound, this is an ultrasonographic diagnosis, there's going to be a thickened prominent pylorus that you can identify. 04:48 And usually with more proximal gastric dilation. 04:51 How do we manage this? So until we can do the operation to open that tight stenosis, we're going to make sure that the infant, it gets adequate fluid replacement. 05:02 We're going to correct any electrolyte abnormalities that hypokalemia that acidosis. 05:09 We're going to restore the acid base balance and try to get the renal parameters more normalized with fluids. 05:17 Surgery, a couple of different approaches. 05:19 So you can do a myotomy, so you can actually go in even endoscopically and cut the smooth muscle and hopefully that will cause sufficient relaxation that you'll no longer have that functional stenosis and obstruction. 05:31 Or you can do an laparoscopic pyeloplasty where you actually go in and dilate the very tight stenosis. 05:39 Okay, not a super common entity, but one that you need to recognize in the pediatric population as an important pathology associated with gastric outlet obstruction. 05:51 And we'll conclude here.
About the Lecture
The lecture Hypertrophic Pyloric Stenosis by Richard Mitchell, MD, PhD is from the course Disorders of the Stomach.
Included Quiz Questions
What is the most common age group affected by hypertrophic pyloric stenosis?
- Infants
- Teenagers
- Preschoolers
- Young adults
- Geriatric patients
What is a common initial symptom of pyloric stenosis?
- Regurgitation after feeding
- Nonbilious projectile vomiting
- Bilious projectile vomiting
- Periumbilical mass
- Weight loss
What is a treatment option for pyloric stenosis?
- Pyloromyotomy
- Pfannenstiel incision
- Whipple
- Cholecystectomy
- Abdominoperineal resection
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Very nice I like your way of teaching Thanks for you very much for the information you provided