Playlist
Show Playlist
Hide Playlist
Hereditary Hemochromatosis: Clinical Presentation, Diagnosis, and Treatment
-
Slides GIP Hereditary Hemochromatosis.pdf
-
Reference List Pathology.pdf
-
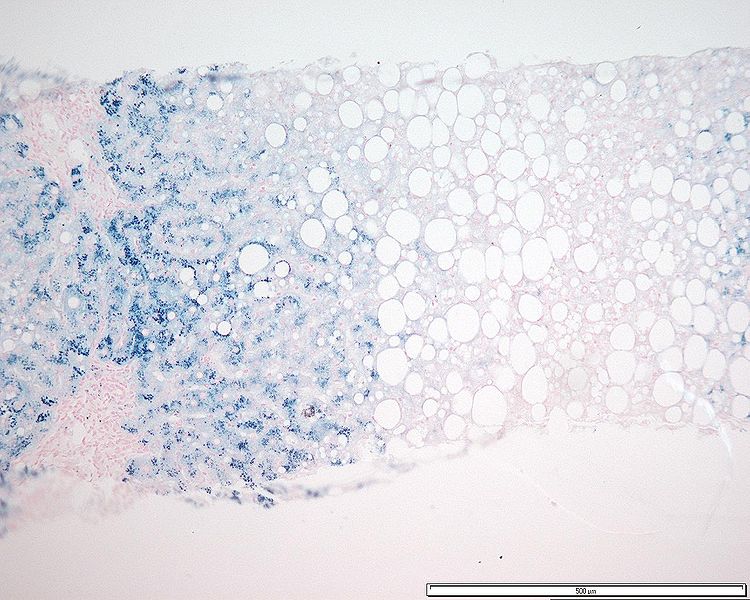
Download Lecture Overview
00:01 The clinical presentation for HH. 00:04 It depends on the tissues that are accumulating the iron, and it depends on degree of iron accumulation. 00:11 In most cases, and certainly at low levels of iron accumulation, it's totally asymptomatic. 00:17 However, with severe disease or chronic late disease, the classic triad is cirrhosis, because now we've caused liver oxidative stress to the point that we have caused irreversible liver damage. 00:30 You will damage the pancreas and particularly the endocrine portion of the pancreas, so that you get iron accumulation that is seen grossly as a bronzing of the tissue, but the patient presents with diabetes. 00:42 You can also get iron accumulation in the skin, and it's called skin bronzing with kind of an increased pigmentation. 00:50 This classic triad doesn't happen so much anymore, simply because we do a much better job of identifying patients with HH and preventing the abnormal accumulation of iron. 01:02 So here are a variety of other tissues that can be affected by iron accumulation. 01:08 Again, the pituitary, the liver and certainly with cirrhosis, you're now at increased risk for a hepatocellular carcinoma. 01:16 You get the pigmentation in the skin otherwise called melanoderma. 01:20 Accumulation in the heart can lead to a arrhythmias and cardiac failure. 01:24 We've already talked about diabetes mellitus, and you can get joint pain you can get osteoarthritis, but also osteoporosis because the trade off between bone resorption and bone synthesis is dysregulated when you have too much iron. 01:39 How do we make the diagnosis. 01:42 It is a bit of a laboratory test in addition to some of the clinical findings, but mostly laboratory. 01:47 So you will see that there is excessive transferrin saturation ever transferrin is how we're going to move, move the iron around the body. 01:54 So we have the total ratio of serum iron to the total iron binding capacity, how much iron could theoretically be bound to all the transferrin. 02:03 If that ratio is above 45%, that suggests that you probably have hemochromatosis, if it's greater than 60%. 02:12 In men, 50% and women it's highly specific for the diagnosis. 02:16 Elevated serum irons 150 micrograms per deciliter, also quite indicative of hemochromatosis, and the total iron binding capacity will tend to also increase and so that in association with a serum iron, and certainly the ratio are going to be things that lead you to your final diagnosis. 02:35 You will also see elevations in serum ferritin. 02:38 Remember ferritin is the storage form of iron within macrophages and within hepatocytes and also other cells around the body. 02:46 When they die, they release that ferritin in a form that we can measure. 02:51 There may be suddenly elevated liver function tests, so you will transaminase that are elevated but they may not be quite so severe as in other forms of liver injury such as hepatitis. 03:04 Once we think we have made a tentative diagnosis, we can be confirmatory by looking for the specific common mutations in the HFE iron sensing genes. 03:15 And homozygosity or heterozygosity for the combined mutations is pretty much diagnostic for hereditary hemochromatosis, and certainly you would want to screen all first degree relatives because if we identify the disease, we can prevent the long term pathologic complications. 03:35 In terms of other diagnostic approaches, imaging, probably not so helpful. 03:40 But a cardiac or hepatic MRI may give you a sense of the degree of iron accumulation and also certainly cardiac function. 03:48 Echocardiogram is going to be important for seeing whether or not you have a dilated or a fibrotic cardiomyopathy, and then biopsy can be the final way to establish this. 04:00 You would do it as typically a core liver biopsy is indicated here. 04:03 And we have specific stains for iron called a Prussian blue stain, and when it's positive, it is a very pretty peacock blue. 04:14 How are we going to manage our patients? So you restrict or limit the amount of iron that they're taking in and this can be both heme iron as well as elemental iron. 04:25 A treatment of choice is recurrent phlebotomy, you simply get rid of a lot of iron by drawing blood. 04:33 The red cells are completely normal, there's nothing wrong with that blood, it can be used for transfusions of somebody else. 04:39 But it's a way to very safely and recurrently remove a fair amount of iron. 04:44 And you can also give drugs that chelate iron that bind up circulating free iron. 04:50 And that's another way to limit the amount of potential damage. 04:53 Other things that we have to be thinking about are the other tissues within the body that are going to be affected by too much iron. 05:02 So we need to do when there's bronze diabetes, when we've affected the endocrine organs, the islets of Langerhans and the ability to make insulin within the pancreas, we need to treat diabetes, we would want to treat in any cirrhosis that develops including things associated with that such as ascites. 05:22 For cardiac failure and arrhythmias, we can give medications that will limit the consequences of that. 05:28 For pituitary involvement, we can give hormone replacement. 05:32 And we want to screen also for paracellular carcinoma, especially when the patient may have evolved to the point where they have cirrhosis. 05:41 Overall with treatment, such as recurrent phlebotomy, the five year survival rate is reasonable, 89%. 05:50 And particularly if the patients don't have cirrhosis, they will be expected to have a completely normal life expectancy. 05:58 That makes the point that if we diagnose this early and we prevent the accumulation of iron and we prevent the accumulation of the secondary consequences of too much iron in various tissues, people can live perfectly normal lives. 06:13 Once liver cirrhosis sets in however, it is irreversible and hepatocellular carcinoma is a known late sequela. 06:21 When patients do die as a result of hemochromatosis, it's cardiac, hepatic, and hepatocellular carcinoma, in terms of the modes of exodus from this world. 06:33 With that, we've covered hereditary hemochromatosis and hopefully you've learned a little bit about iron metabolism, iron absorption and its regulation.
About the Lecture
The lecture Hereditary Hemochromatosis: Clinical Presentation, Diagnosis, and Treatment by Richard Mitchell, MD, PhD is from the course Disorders of the Hepatobiliary System.
Included Quiz Questions
What is the classic triad of late symptoms of hereditary hemochromatosis? Select all that apply.
- Cirrhosis
- Diabetes
- Skin bronzing
- Splenomegaly
- Ascites
Which of the following laboratory findings is consistent with hereditary hemochromatosis?
- Tf saturation of 70%
- Iron level of 100 mcg/dL
- Iron level of 85 mcg/dL
- Decreased serum ferritin
- Decreased ALT
What is the treatment of choice for hereditary hemochromatosis?
- Phlebotomy
- Dietary restriction
- Metformin
- Amlodipine
- Paracentesis
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |