Playlist
Show Playlist
Hide Playlist
Giant Cell Aortitis and Takayasu Arteritis
-
Slides Vasculitis Mitchell.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
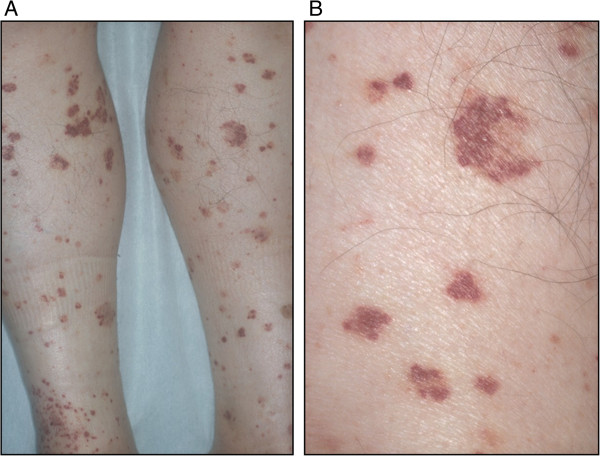
00:01 Okay, here's the later. We've talked about the basic mechanisms that gives you way to think about how this happens, how these happen, now we're talking about the specifics. 00:10 And each one of these vasculitides will have kind of a different presentation, will have different outcomes, will have different kind of epidemiology, and those are the sorts of things they like to test on the board exam. 00:24 So, you have to kind of make a table and think your way through all the little specifics, because there are lots of little specifics. 00:32 So, giant cell aortitis and Takayasu's arteritis are actually very similar. 00:38 In fact, identical in terms of their pathologic appearance. 00:42 They are a granulomatous, so a T cell driven vasculitis of large to medium-sized vessels of the aorta and the main branches. 00:50 An important point, and this is just an epidemiologic point, they are identical histologically. 00:57 If you show me a slide of a giant cell aortitis in the aorta and a slide of a Takayasu's aortitis or arteritis, I couldn't tell them apart. 01:07 But epidemiologically, if someone has the same pathology in a large vessel and they're under the age of 50, we say it's Takayasu. 01:17 And if they are older than 50, we say they had giant cell. 01:20 That's the main difference. Takayasu's has classically been associated with the Asian heritage. 01:28 It was originally described by Dr. Takayasu, but in fact, it has a very global distribution. 01:34 It is not restricted to the Asian population. 01:37 These arteritis, Takayasu's and giant cell, are both more common in women overall. 01:44 And we're just looking at examples. On the left-hand side is a giant cell aortitis. 01:49 Giant cell aortitis tends to involve more of the aorta than it does of the great vessels of the arch. 01:56 It tends to cause a thickening of the wall, and with damage to the wall, we get dilation. 02:02 So, this is a dilated aorta with a thickened wall. 02:06 On the other hand, Takayasu arteritis tends to involve the next levels down in size of the vessel. 02:14 So, it's not the aorta. It tends to involve the vessels of the arch, the great vessels. 02:19 So, the innominate, subclavian, carotid, et cetera. 02:24 And you see on the right-hand side highlighted by a red oval is an area where we have relative stenosis there of the left subclavian artery coming off on this patient. 02:36 There will also, in this particular case, appears to be left carotid as well. 02:42 And there's less flow of the radiocontrast dye. 02:45 What does it look like? I'm showing you kind of normal on the left-hand side. 02:52 It's a stain for elastic tissue, and slightly different background stain, but the same elastic tissue stain. 03:01 The normal laminations in a normal aorta are well-layered throughout and are uniform. 03:06 In a giant cell aortitis, there has been large scale destruction of vast swaths of the media, and destruction of the elastic tissue. 03:18 And we see at the margins of these areas of destruction, granulomatous inflammation, giant cells, activated macrophages. 03:26 There's going to be a lot of medial smooth muscle necrosis and destruction as a result of the inflammatory cell recruitment. 03:33 And because now we have damage to the media, we're going to have dilation of the vessel, the response, including the activation of smooth muscle cells because of the damage is that we will get intimal hyperplasia, a thickening and relative stenosis of the affected blood vessels. 03:49 In the aorta, not so much of a problem. 03:52 But in a subclavian artery, a big problem is that gets narrowed, and one of the other names for Takayasu's is pulseless disease, as we'll see in a subsequent slide. 04:05 So, science and symptoms of a Takayasu's arteritis, again, going to be more likely to involve - not exclusively, but more likely to involve the vessels of the arch, the great vessels. 04:15 So, not specific symptomatic things due to cytokine elaboration. 04:20 Systematically - systemically is going to be fever, malaise, arthralgias, and night sweats. 04:25 These are nonspecific. The vascular symptoms, because of the narrowing of the vessels, that you get syncope. Patients will actually lose consciousness. 04:36 They can also have involvement of the coronary arteries, so they can get angina. 04:40 Because of the narrowing of the carotid, you will hear bruits. 04:45 So, if you put a stethoscope there, you'll hear a swooshing sound, and there will be a weak pulse depending on the degree of stenosis due to the intimal hyperplasia. 04:54 Involvement of the ophthalmic arteries will give you visual field defects. 04:59 Because of the narrowing of the vessels going out to the extremities, so the larger vessels, the subclavians for example, you'll get a Raynaud's phenomena, which is being demonstrated in the image on the right. 05:12 Skin manifestations include erythema nodosum. 05:15 So, nonspecific inflammatory consequences of having systemic cytokine elaboration. 05:23 And as noted in the red box at the bottom, Takayasu's arteritis is known as pulseless disease because of the involvement of those large arch vessels. 05:33 Giant Cell Arteritis tends to have some of the same systemic manifestations fever, malaise, arthralgias, a night sweats due to systemic cytokine elaboration. 05:42 Tthey may have back or abdominal pain depending on degree of involvement of the aorta. 05:47 There is upper and lower extremity claudication with pulse deficits. 05:51 This is less common than in Takayasu's but can occur. 05:54 And again, although we talk about Takayasu involving the great vessels of the arch, giant cell arteritis involving the aorta, there's a lot of overlap between the two.
About the Lecture
The lecture Giant Cell Aortitis and Takayasu Arteritis by Richard Mitchell, MD, PhD is from the course Vasculitis.
Included Quiz Questions
What age group is associated with giant cell arteritis?
- > 50 years
- < 50 years
- > 70 years
- < 70 years
- < 30 years
Which vessels are most affected by Takayasu arteritis?
- Large arteries
- Arterioles
- Capillaries
- Small arteries
- Small vessels
What skin manifestation is associated with Takayasu arteritis?
- Erythema nodosum
- Erythema multiforme
- Erythema toxicum
- Erythema marginatum
- Erythema migrans
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |