Playlist
Show Playlist
Hide Playlist
Gastric Cancer
-
Slides GIP Gastric Cancer.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
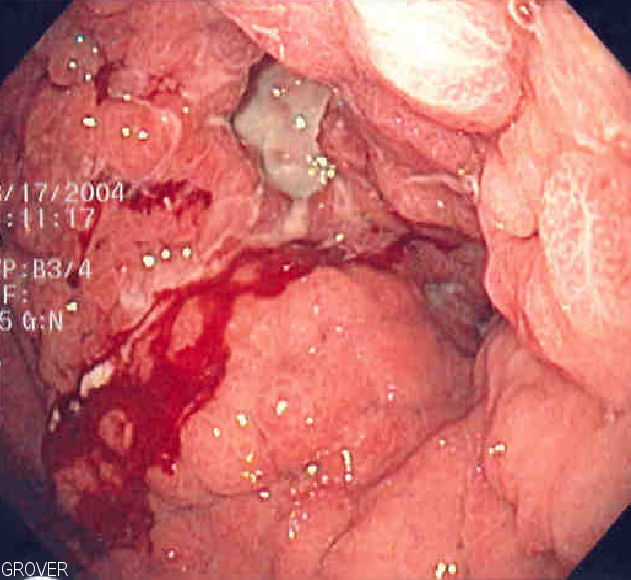
00:01 Hello and welcome. 00:02 In this talk, we're going to cover gastric carcinoma, cancer of the stomach. 00:08 Let's talk about epidemiology first. 00:10 So although it is clearly not the most common malignancy in the world, it is the third most common cause of cancer related death worldwide. 00:19 So it is a bad actor. 00:21 If you have gastric cancer, that's not usually a good prognosis. 00:26 There is, interestingly enough, a higher incidence in certain parts of the world. 00:30 This is not uniformly distributed around the world, although, as we'll talk about, some of the causative factors are relatively common, such as Helicobacter pylori. 00:40 But it's more common in eastern Asia, and Eastern Europe and South America. 00:45 Some of this is related to genetics. 00:48 Some of it is related to dietary commonalities in terms of what gets ingested, such as nitrosamines and food. 00:57 And some of this is related to infections, common infections, such as Helicobacter. 01:04 Overall, gastric cancer occurs more frequently in men than in women. 01:09 And the reasons for that are not exactly understood. 01:13 The median age at the time of diagnosis is usually in the seventh decades. 01:17 So typically, older individuals, men more common than women. 01:21 The majority of the gastric cancers, cancers of the stomach are going to be Adenocarcinoma. 01:27 So these are big gland forming cancers. 01:31 There can be two types. 01:33 One is the intestinal type, which tends to be nodular and quite focal, that's the majority 70% or so of patients will have that. 01:40 And the typical location for that is down near the pylorus in the antrum of the stomach, although it can occur in other places. 01:49 That's going to be the one that's more common in men, older age groups, and lower socioeconomic classes probably related to infectious etiologies, again, such as Helicobacter. 02:00 There's a second type, which is about a third overall of these Adenocarcinomas. 02:07 And that's going to be the linitis plastica type that's literally translated as a leather bottle. 02:12 I'll show you what that looks like on the next slide. 02:15 This has an equal sex distribution, and it tends to be a much more infiltrative diffuse tumor. 02:21 So it doesn't have focal nodules. 02:23 It's kind of diffusely infiltrative. 02:26 And it's more common in younger age groups. 02:28 So that's kind of the epidemiology. 02:31 There are other cancers that we're not going to spend too much time talking about that's about 13% of the overall gastric cancers are actually lymphomas, not epithelial malignancies, not carcinomas. 02:43 The stomach is the most common extranodal site of lymphomas, that's because there's lots of inflammation in the stomach. 02:50 And with driving inflammation, we will have local nodal hyperplasia of lymphocytes, and they may acquire over time certain mutations that allow them to become mucosal associated lymphoid tissue tumors or MALT lymphomas. 03:04 Those will transform eventually to a large cell lymphoma. 03:08 The MALT as you might expect, is associated with inflammation not otherwise specified, but specifically with Helicobacter pylori which drives a very prominent inflammatory response. 03:18 And then there are the non-epithelial non-carcinoma gastric cancers, such as the gastrointestinal stromal tumor or GIST which is about 1% of primary gastric cancers. 03:28 This is a tumor of the cells interstitial cell of Cajal which are cells that are responsible for maintaining normal peristaltic activity. 03:38 They're relatively rare kind of gastric cancers, but ones that is necessary that we specifically identify because treatment is targeted to unique mutations that occur in these tumors. 03:54 And then finally, carcinoid tumors. 03:56 And these are relatively rare. 03:58 They're very slow growing. 03:59 They're neuroendocrine tumors. 04:01 They tend to have a much more indolent course. 04:04 So we've talked about the other ones. 04:05 We talked about MALT lymphomas and the GISTs and the carcinoid. 04:10 We're really going to focus here on the carcinomas, epithelial malignancy. 04:15 Let's talk about pathophysiology. 04:17 So risk factors for gastric carcinoma is inflammation of the stomach. 04:23 And so anything that will cause inflammation of the stomach which causes mucosal damage, and inflammation which is going to release a variety of cytokine mediators and reactive oxygen species is going to drive the production of epithelial tumors. 04:39 So gastroesophageal reflux disease or GERD is going to be a cause. 04:44 Obesity in general is associated with this that may actually reflect a certain amount of reflux disease. 04:50 Remember that obesity is a risk factor for GERD. 04:54 Processed foods, more nitrosamines, so things that are in the diet can also impact the development of gastric carcinoma. 05:02 Clearly Helicobacter pylori infection and I've already mentioned about five times, so it's probably important cause. 05:09 Gastritis not otherwise specified any inflammation of the GI lining, of the stomach lining will cause increased risk. 05:16 Smoking. 05:17 Because smoking reduces the mucus production which will be an increased risk for gastritis. 05:23 Bile reflux. 05:24 So normally, the bile is released into the first part of the duodenum, second part of the duodenum and goes more distal. 05:33 Sometimes that can reflux through the pylorus into the stomach. 05:37 And bile can be an irritating agent, but can also induce the production of inflammatory mediators. 05:45 And then there are a variety of genetic underpinnings for gastric malignancy. 05:50 So hereditary nonpolyposis, colorectal cancer, abbreviated HNPCC, or familial adenomatous polyposis. 05:58 Those specific mutations associated with those entities can give you an increased risk of gastric cancer as well as epithelial malignancies elsewhere in the GI tract. 06:09 So this is just a schematic kind of a cartoon to give you a sense of the basic mechanism by which injury in quotation marks not otherwise specified can ultimately cause malignancy. 06:20 So we have injury, it could be Helicobacter, it could be smoking, it could be a whole variety of things that cause inflammation and injury. 06:29 An injury will cause loss of cells. 06:32 And to replace those cells, we make more cells. 06:35 So we have proliferation ongoing. 06:38 So we have now new DNA being synthesized. 06:41 At the same time that injury has also elicited the recruitment of inflammatory cells, macrophages, neutrophils, T lymphocytes. 06:50 Those cells are making a variety of mediators that are part of inflammation, including reactive oxygen species. 06:57 Reactive oxygen species will cause mutations can cause DNA breaks, for example. 07:04 And now we can have DNA breaks occurring in the setting of proliferating cells. 07:10 That's a recipe for the development, or for the generation of mutations that get permanently locked into the genome. 07:19 So we'll acquire cellular mutations. 07:21 Oops, now we're on our way to malignancy and invasive cancers. 07:27 So I've talked about the intestinal type. 07:30 I just want to spend a moment talking about the diffuse type. 07:33 Linitis plastica, a Latin phrase meaning leather bottle. 07:37 On the left hand side, you see an example of a leather bottle. 07:40 It used to be the way that the ancient Romans would transport their various liquids in a leather pouch like that. 07:49 The thickness and kind of the diffuse kind of thickening of the wall is what gives it that leather bottle appearance. 07:56 So this is that infiltrative tumor. 07:59 So it's associated more commonly, not so much with the typical inflammatory mediators that we just talked about, but by specific mutations. 08:07 And in particular, we see loss of function mutations in CDH1, that's a tumor suppressor gene, that is encoding the adhesion protein E-cadherin. 08:17 Loss of that leads to ongoing proliferation, and it tends to give rise to that diffuse infiltrative tumor. 08:26 This is just showing you example of what this looks like. 08:28 So the tumor cells are I highlighted here with green circles. 08:32 They are adenocarcinoma so they have mucin within them, and they tend to be kind of sneaky. 08:38 They are infiltrating and inducing the local tissue around them to produce a fibrosis that's how we get that thick leather bottle sort of appearance grossly. 08:49 So the clinical presentation of cancers of the stomach. 08:55 In the early stages, as you might expect, it can be asymptomatic. 09:01 As we develop symptomatology that usually suggest much more advanced cancer. 09:06 And the main reason it's the third leading cause of cancer mortality in the world is that it usually is discovered at a stage where it's much more advanced. 09:15 So the symptoms suggesting worse kind of prognosis and more advanced disease include epigastric discomfort actually feeling like there is a a mass or a pain there. 09:28 A combination of the tumor and some of the factors that it makes, as well as just pressure at that spot, the patient may develop anorexia, doesn't feel like eating, there may be nausea. 09:42 There may be weight loss as a result of not eating and not having good flow of food, nutrition through the stomach and into the rest of the GI tract. 09:55 As we get further along, there's going to be increasing levels of nausea. 10:01 To the satiety becomes even earlier and earlier, very little food will make you feel like you're completely full. 10:07 You may have a formal outlet obstruction, and in that case may have vomiting after ingesting food. 10:13 And as the tumor erodes and and undergoes focal necrosis itself, you may develop either vomiting of blood, hematemesis or you may have Melena, you may have dark tarry stools representing bleeding into the GI tract that eventually comes out at the distal end. 10:33 The signs overall, there may be a completely normal physical exam or there may be an epigastric mass. 10:40 Other signs, particularly of metastatic disease, you may have an enlarged liver, a palpable liver mass or a very irregular margin underneath the right upper quadrant underneath the ribcage. 10:56 A Virchow's node is the node that sits right at the junction of the thoracic duct and left subclavian vein. 11:06 And it is about right there, an enlarged node. 11:08 There is classic for gastric carcinoma. 11:11 For reasons I don't understand an Irish node can occur in the left excellent again drainage presumably from lymphatics coming of a gastric cancer. 11:22 You can have a Sister Mary Joseph's nodule which is actually going out old umbilical vein connections so that you get a periumbilical nodule of tumor and the tumor may slough on the surface of the stomach and/or may have increased vascular permeability and then you will develop in a sideways. 11:42 Paraneoplastic findings. 11:44 And these are not unique to gastric carcinoma, they occur in a variety of carcinomas. 11:49 But you can get a acanthosis nigricans kind of a soft, velvety hyper pigmented cutaneous lesion. 11:56 This is due to keratinocyte activation and proliferation. 12:01 You can get multiple seborrheic keratoses, a dermatomyositis, so autoimmune inflammatory disease may happen. 12:09 Hypercoagulable states are very common particularly with the adenocarcinomas at a linitis plastica of variety and a membranous nephropathy usually due to immune complex deposition. 12:20 Diagnosis. 12:22 So in patients who are high risk, that is to say patients with familial adenomatous polyposis, hereditary nonpolyposis colorectal cancer and others, we will constantly surveil and hopefully pick up malignancy by doing endoscopy, an earlier stage and be able to intervene. 12:41 Patients who have a prior history of gastric adenomas, little benign proliferations of the gastric epithelium are also at high risk. 12:50 If there has been a prolonged history of gastritis, whether it's atrophic or not, that chronic inflammation hitting the gastric epithelium is going to put the patient at increased risk. 13:03 And then we've already identified certain high risk ethnic populations, Eastern Asian, Eastern European and South America. 13:11 Our main diagnostic modality is going to be esophagogastroduodenoscopy, EGD. 13:18 And we're going to look for ulcerated masses, irregular heaped up margins, and induration. 13:25 And in linitis plastica, it actually may be much more subtle. 13:29 Remember, just had those sneaky little cells kind of going throughout the wall. 13:34 But what we'll see is the wall is very stiff. 13:37 So it doesn't really descend appropriately. 13:41 And we may not see really good rugal folds, for example in the stomach. 13:45 Overall, unless you have a really deep ulceration associate with the tumor, barium imaging has much lower sensitivity and you really want to do an EGD. 13:56 How are we going to manage this? Well, I already told you, the vast majority of patients are going to present later in the course. 14:02 So, although we can do surgery, although we can do chemotherapy, those are not in general going to give us a very happy outcome. 14:12 So, if Helicobacter pylori is a driving force in this, you can definitely do that. 14:18 But at the point you've made the diagnosis of cancer, additional Helicobacter pylori therapy is not going to make a huge difference. 14:26 The clinical staging is going to be very important for dictating our therapies. 14:31 So if it's non metastatic, usually or more commonly, you will have a successful outcome with chemotherapy and surgery. 14:40 With metastatic disease, our chemotherapies are usually not going to be successful. 14:47 And you may do a palliative gastric resection just to prevent obstruction or severe bleeding. 14:53 But chemotherapy and radiation, everything else you're going to do is usually not going to have a good outcome once we have metastatic spread. 15:00 So the overall 5-year survival is 30%. 15:03 I already said this is a bad actor, the third leading cause of cancer mortality in the world. 15:10 Even with curative surgical resection where we got it all, the patients are about 50/50 in terms of their 5-year survival. 15:20 And the stages that are there. 15:21 So local disease, local disease of a certain size, local disease with nodal spread or distant disease stages 1-4, you can see the survival curves and overall not a happy outcome. 15:39 So unfortunately, not super uplifting topic, but one, especially in large portions of the world we need to pay attention to. 15:49 I hope you've enjoyed the talk on gastric carcinoma.
About the Lecture
The lecture Gastric Cancer by Richard Mitchell, MD, PhD is from the course Disorders of the Stomach.
Included Quiz Questions
What is the most common histology of gastric cancer?
- Adenocarcinoma
- Squamous cell carcinoma
- Epithelioid carcinoma
- Sarcoma
- Lymphoma
What is the most common type of gastric adenocarcinoma?
- Intestinal type
- Diffuse type
- Antral type
- Pyloric type
- Body type
What are the initial 3 pathophysiologic steps leading to gastric cancer?
- Injury, inflammation, proliferation
- Injury, proliferation, mutations
- Proliferation, mutations, invasive cancer
- Injury, mutations, invasive cancer
- Inflammation, mutations, proliferative cancer
What is NOT a typical symptom of gastric cancer?
- Constipation
- Epigastric discomfort
- Anorexia
- Nausea
- Weight loss
What is a possible sign of gastric cancer?
- Virchow node
- Splenomegaly
- Scottish node
- Sister Mary Timothy nodule
- Rheumatoid arthritis
What is the preferred diagnostic test for gastric cancer?
- EGD
- Colonoscopy
- CT abdomen
- MRI abdomen
- Abdominal ultrasound
What is the typical treatment for nonmetastatic gastric cancer?
- Chemotherapy and surgery
- Chemotherapy
- Surgery
- Radiation and chemotherapy
- Radiation and surgery
What is the five-year survival of gastric cancer?
- 30%
- 5%
- 60%
- 15%
- 90%
Customer reviews
4,0 of 5 stars
| 5 Stars |
|
2 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
1 |
| 1 Star |
|
0 |
3 customer reviews without text
3 user review without text