Playlist
Show Playlist
Hide Playlist
Gallstones: Risk Factors, Types & Clinical Presentation
-
Slides Pancreas and Biliary Tract.pdf
-
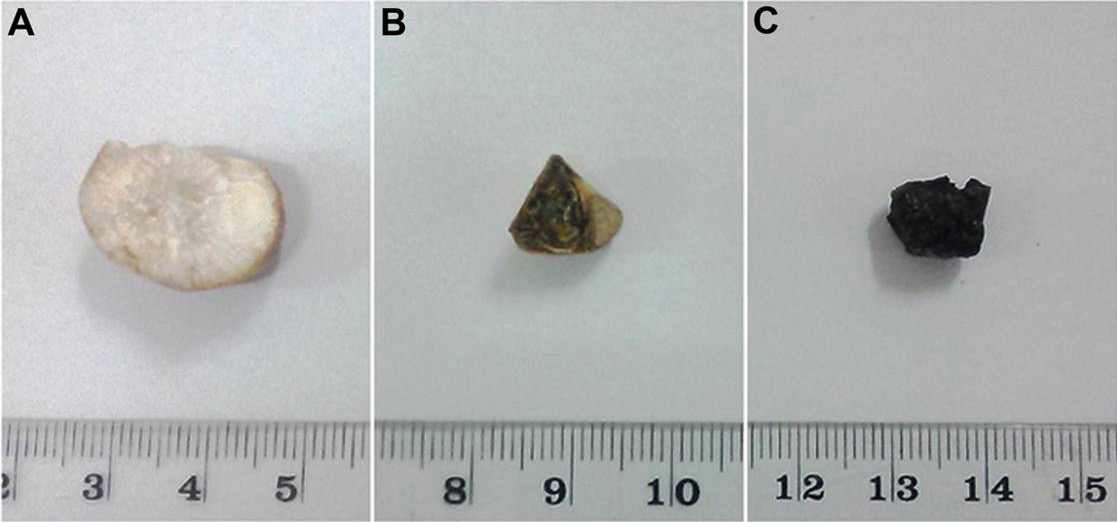
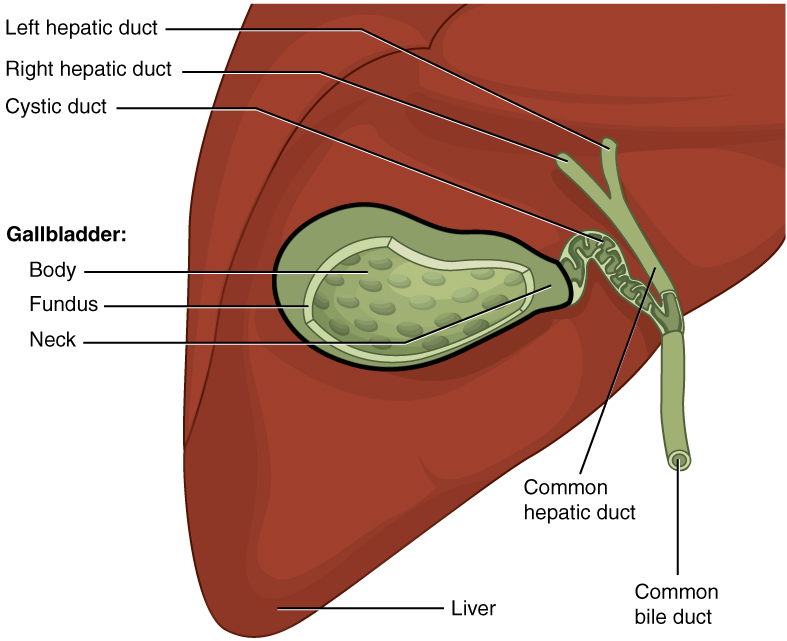
Download Lecture Overview
00:01 Gallstones is where we’re at. There might be a genetic predisposition. 00:06 If you see the letter F or derivatives of, is your patient a woman, a female, F? Is she in her reproductive age, fertile? Is she pregnant? Is she fat? Female, forty, fat, fertile, FFFF. 00:32 The type of gallstone that you’re thinking, when the F criteria have been met, cholesterol, the most common. 00:40 Now, with all that said, be careful though, okay? You want to take a look at the history of your patient. 00:46 If there’s a history in which there’s bilirubin, let’s say for example, sickle cell disease, how much bilirubin is being released? Whew, a lot, right? And if it’s bilirubin that is accumulating, giving rise to a stone in the gallbladder, why would you call that a cholesterol stone? Do you see what I’m saying? So percentage-wise, sure, as long as you meet the criteria, but be careful. 01:09 Pay attention to history. 01:12 Risk factors; octreotide, ceftriaxone, OCP, prolonged TPN, and ileal disease causing bile acid malabsorption. 01:22 For example, remember where intrahepatic circulation takes place? In the terminal ileum. 01:29 If there are indications for, perhaps, for removing parts of terminal ileum, there’s every possibility that results in bile acid malabsorption. 01:37 Therefore, increases of the risk of gallstones cholesterol type. 01:43 Two types, the type we just talked about, cholesterol -- FFFF, female, forty, fat, fertile. 01:52 Pigment, I gave an example, Sickle cell disease, increased extravascular hemolysis. You have unconjugated bilirubin, and the bilirubin may also accumulate within the gallbladder. 02:06 With the gallstone, what’s the kind of pain that the patient's going to feel? Postprandial. 02:13 What kind of meal? “Hey, doc. I just had a cheeseburger.” Great. 02:17 "After a cheeseburger, how did you feel?” “Whoa, a pain. Shooting right here, right upper quadrant." On a scale of one to ten, with ten being the worst pain that the patient has experienced, the patient feels pain at eight or nine. 02:34 Pretty sharp, isn’t it? Pretty sharp. 02:37 Biliary colic is what this will be referred to as. 02:41 Topic: gallstone, presentation that you’re looking at. 02:44 But because of the obstruction, the patient is going to have right upper quadrant pain. I told you it was a story. 02:51 So we ended up developing a stone. The stone was in the gallbladder. 02:57 Every time there’s contraction, the bile cannot come out. 03:02 Now the stone is making its way to the head of the gallbladder. 03:06 Are you picturing it? Picture that for me. 03:08 There’s my stone. And maybe it’s in the cystic duct right there, Every time there’s contraction, contraction, contraction, contraction, the stone gets in the way, “Ouch, ouch, ouch,” sharp pain, right upper quadrant. 03:22 Now, over repeated bouts of that contraction-obstruction, how do you think the wall of the gallbladder is then going to respond? Inflammation. It has to. This is called acute cholecystitis. 03:37 So move from biliary colic in the previous discussion, with pain, and the gallbladder, my goodness, it’s going to respond, and it’s undergoing inflammation. 03:46 There will be right upper quadrant pain with fever, nausea, and vomiting. 03:49 That’s a lot of pain. 03:52 A sign that you may find on clinical examination of a patient with acute cholecystitis is Murphy’s sign. 03:59 In order to produce the Murphy’s sign, you ask the patient to take a deep breath while you place your hand in the right upper quadrant below the costal margin in the mid-clavicular line. 04:09 Murphy’s sign is considered positive if the patient stops breathing during inspiration. 04:15 Obstructive jaundice is usually not encountered in the context of acute cholecystitis since the common bile duct is typically open allowing the normal flow of bile from the liver to duodenum. 04:27 Obstructive jaundice can occur in Mirizzi syndrome, where the gallstones lodged in the cystic duct or the Hartmann’s pouch externally compress the common hepatic duct, thus obstructing the flow of bile. 04:41 Obstructive jaundice. Think about where you are. Stone, gallbladder duct. 04:48 Of course, it’s obstructive jaundice. 04:51 A rare condition known as Mirizzi's syndrome in which you have adjacent structures such as the common bile duct which is also being affected. 05:02 Acute cholecystitis, acalculous type, meaning to say you might not even have a stone, but yet still results in cholecystitis. 05:12 Critically ill patient, unfortunately, there could be higher mortality in terms of what may happen. Complications include, over a long period of time, if you’ve not corrected this, one would never think that, you know, this has such serious sequelae, but it does. You can’t just allow for bile to remain stasis. 05:30 You can’t. Bile has all kinds of constituents. 05:34 Look for complications, empyema, gangrene, gallstone ileus. 05:38 So from now on, apart from your normal presentation that you’re so accustomed to, understand that you need to take out the stone. 05:48 You need to, maybe perhaps, take out the gallbladder. 05:50 If you don’t, the complications become extremely disastrous. 05:56 Remember that stasis I was talking to you about? If you don’t remove the stone, and maybe perhaps if you don’t correct the issue, at some point in time, infection's going to set in. And when it does, you call this cholangitis. High fever with chills and hypotension, associated with the gram-negative bacteremia. 06:13 Now, critically ill, high mortality. There you are. 06:19 There is a patient undergoing stasis of the bile and such and infection has kicked in with gram-negative organism, bacteremia, keep going, uh-oh, septicemia, sepsis, death. 06:31 See what I’m getting at? It’s a story, but you need to make sure that you know how to deal with this story properly and deal with your patient accordingly. 06:40 Our topic now is still gallstone. I want you to move the stone out of the gallbladder. We talked about cholecystitis, we talked about how that stone caused obstructive jaundice, we talked about infection may set in, may result in cholangitis. 06:57 What if the stone makes its way down? Now picture the anatomy that I walked you through quickly. 07:03 And it comes down the common bile duct. 07:05 Along with the pancreatic duct, they’re supposed to hook up, right? But if you had that stone now here by the common bile duct, not only are you going to have damage to the gallbladder and the tree, you’re also going to have damage to the pancreas. 07:20 Welcome to pancreatitis. 07:22 Acute impaction of gallstone in the ampulla of Vater. Think about where that is. 07:27 Most stones, thank goodness, will pass spontaneously, but there’s every possibility that it might get stuck. 07:33 Urgent ERCP to extract the stone improves the outcome.
About the Lecture
The lecture Gallstones: Risk Factors, Types & Clinical Presentation by Carlo Raj, MD is from the course Pancreatic and Biliary Tract Diseases: Basic Principles with Carlo Raj.
Included Quiz Questions
Which of the following is NOT a risk factor for the formation of gallstones?
- Alcohol
- Being a woman in her 5th decade
- Prolonged total parenteral nutrition
- Obesity
- Ileal disease causing bile acid malabsorption
Which of the following drugs is NOT associated with the development of gallstones?
- Ampicillin
- Clofibrate
- Oral contraceptive pills (OCPs)
- Ceftriaxone
- Octreotide
A 40-year-old woman presents with right upper quadrant pain. She has a history of diabetes and a BMI of 28 kg/m^mirizz2. She complains of feeling nauseated at times. What is the probable type of gallbladder stone causing the right upper quadrant pain?
- Pure cholesterol stone
- Mixed stones
- Combined stones
- Pigment stone
- Uric acid stone
A 10-year-old boy complains of weakness and easy fatigability. It is determined that he has failure to thrive, and on physical exam, frontal bossing is seen. His peripheral smear shows target cells. He also complains of right upper quadrant pain on examination. What type of gallbladder stone is MOST likely causing the right upper quadrant pain?
- Pigment stone
- Pure cholesterol stone
- Mixed stones
- Combined stones
- Uric acid stone
Which of the following describes Mirizzi syndrome?
- External compression of the common hepatic duct by a gallstone in the cystic duct
- Saccular dilatations of the intrahepatic duct
- Hepatic vein thrombosis
- Migratory thrombophlebitis
- Hepatic artery thrombosis
Which of the following is NOT a complication of acute cholecystitis?
- Cholesterolosis
- Gallstone ileus
- Chronic cholecystitis
- Gangrene
Which of the following conditions warrants an urgent ERCP?
- Gallstone pancreatitis
- Gallstone ileus
- Empyema of the gallbladder
- Gangrenous gallbladder
- Obstruction of gallstone at the neck of the gallbladder
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Dr. Raj taught with clinical scenarios in view. I like the fact that he gives acronyms.