Playlist
Show Playlist
Hide Playlist
Gallstones: Diagnosis and Management
-
Slides Pancreas and Biliary Tract.pdf
-
Download Lecture Overview
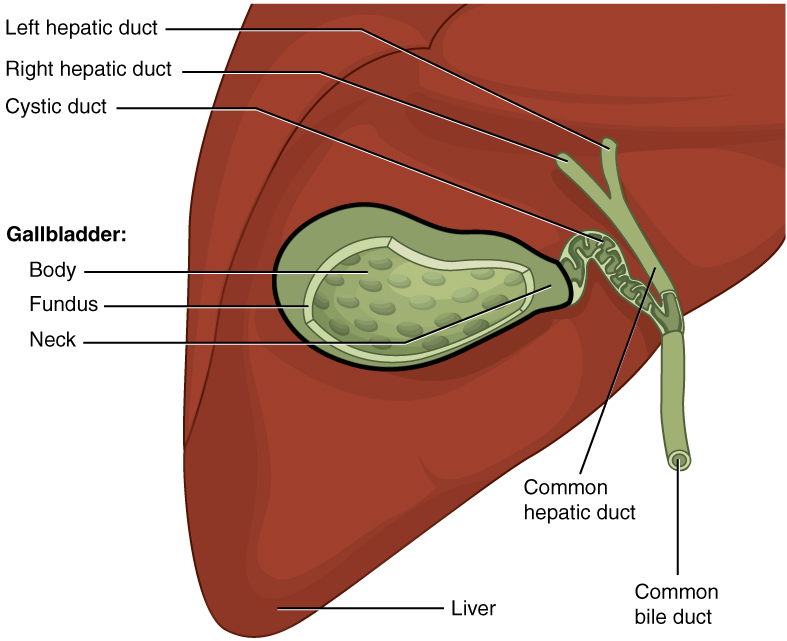
00:01 Imaging. The type of radiology and imaging study that you’d use, ultrasound. 00:06 The gallstones are symptoms that you would find inside my gallbladder. 00:10 In addition, remember, if the gallbladder has been obstructed, you can imagine that the gallbladder wall has become inflamed. Therefore, you’d expect to find thickening and edema of the gallbladder wall. 00:21 In fact, histologically, when the gallbladder has become thickened and cholecystitis continues, at some point in time -- have you heard? I know that you have. In medical school and during your education, you’ve heard of something called porcelain gallbladder. 00:39 What color is porcelain? White. 00:42 Gallbladder is not that color normally. So what is then contributing to the whitishness of the gallbladder, the porcelain? The thick wall at some point might start eroding. 00:55 If you have erosion, there's s a term, that will be called or known as Rokitansky, Rokitansky type of sinus. And with that Rokitansky type of sinus that develops, you might have calcium accumulating, and this is dystrophic calcification. 01:15 Calcium is what color? White. 01:17 Ultrasound will show you gallstones in the gallbladder, thickening of that wall with edema. And you have something called your dilated biliary tree. 01:27 You’re going to like this one. You’re going to bring in some anatomy, you’re going to know some physio, and we’re going to use pathology so that we can use something called a HIDA scan. Pay attention. 01:43 Stone, gallbladder, think about what that is. 01:48 Contraction, obstruction, cholecystitis, maybe Rokitansky type of sinus that we talked about. 01:56 Ultrasound is going to help you identify the gallstone. 01:59 Now, here’s my problem. I don’t find a stone. 02:03 Oh, boy. I don’t find a stone perhaps in the gallbladder. 02:07 But you know there’s obstruction based on the symptoms of your patient. 02:11 But you don’t know where the stone is. 02:13 You don’t know if the stone is located in the cystic duct or if the stone is down the common bile duct. 02:20 If you’re not clear about this anatomy, I mentioned this earlier, I asked you kindly to make sure that you’re familiar with at least the basic anatomy here to walk us through these type of imaging studies that you’ll be asked about on your boards. 02:34 Your HIDA scan. Remember, from the liver is where bile synthesis takes place. 02:41 It will be taken to the bile duct in the liver, out of the liver, and into the gallbladder, normally. 02:48 What if you had a method by which you injected a dye, hepatic endo-diacetic acid. 02:55 You had a dye. HIDA stands for hepatic endo-diacetic acid. 02:59 Do not worry about the name per se. 03:01 It’s the dye that you’re putting into the liver. 03:04 You’re going to radiographically follow the dye and see as to whether or not it should end up in your gallbladder. Are you with me? What if the stone is in the cystic duct? Go back and take a look at the anatomy. 03:19 If that stone is in cystic duct, is that dye going to make its way from the liver to the gallbladder? No. 03:31 Therefore, useful in doubtful cases of cholecystitis, because this will tell you if the cholecystitis was being caused by a stone in the cystic duct. And if the dye doesn’t make it in the gallbladder, this confirms that your stone and the cholecystitis was caused by the stone in the cystic duct. 03:52 It couldn’t be any clearer than that. If that still remains confusing, go back and review what I just said here because that part, I guarantee, you’ll be asked about that in some way, shape, or form. 04:04 Ultrasound, HIDA scan. Ultrasound of the gallbladder. 04:10 That arrow that we’re seeing here on the ultrasound is actually showing you a stone within the gallbladder. 04:17 Let's talk about the management of what made it happen when the gallstone, if there's a gallstone resulting in cholecystitis. 04:26 Let's talk about a further detail about each one of these steps and management here. 04:31 Cholecystectomy, not recommended for asymptomatic disease or in setting of acute cholecystitis. 04:38 You wanna try to avoid surgery as much as possible if the patient is asymptomatic and acute cholecystitis, since to whether you're not able to manage your patient conservatively. 04:48 There's elective surgery which then -- with significant lower complication rate, cholecystectomy. 04:55 What if he had a patient who's unable to perform or wasn't eligible for cholecystectomy because of being critically ill and then cholecystitis is not being the cause by a stone, we call this acalculous cholecystitis. 05:12 So if it's acalculous cholecystitis, maybe due to infection, and the patient is severely ill and contraindicated for having surgery, then obviously cholecystectomy cannnot be done. 05:24 Well, with infection being a common cause of acalculous cholecystitis and IV antibiotics and hydration would be recommended. 05:34 If the patient wouldn't be able to tolerate cholecystectomy, then percutaneous drainage for the acalculous cholecystitis would be recommended. 05:43 Remember what this acalculous cholecystitis mean, inflammation of the gallbladder taking place not due to a gallstone but maybe perhaps due to some type of infection. 05:53 Endoscopic retrograde cholangiopancreatography, an urgent procedure for decompression with sphicterotomy. 06:01 This will be some of the steps that you wanna keep in mind when dealing with the management of cholecystitis.
About the Lecture
The lecture Gallstones: Diagnosis and Management by Carlo Raj, MD is from the course Pancreatic and Biliary Tract Diseases: Basic Principles with Carlo Raj.
Included Quiz Questions
A patient has pain on the right side of the abdomen radiating to the right shoulder. The serum transaminases, alkaline phosphatase, and serum lipase are increased. Which location is the MOST likely site of impaction of the stone?
- The stone is present at the sphincter of Oddi.
- The stone is impacted at the cystic duct.
- The stone is impacted at the left hepatic bile duct.
- The stone is impacted at the right hepatic duct.
- The stone is impacted at the neck of the gallbladder.
Which of the following conditions carries an increased risk of gallbladder cancer?
- Porcelain gallbladder
- Gallbladder with gallstone
- Acute cholecystitis
- Chronic cholecystitis
- Cholesterolosis of gallbladder
Which of the following examination findings are associated with a diagnosis of cholelithiasis?
- Abdominal tenderness and pain radiating to the right shoulder
- Abdominal tenderness and pain radiating to the left shoulder
- Pain when the examiner releases the hand after applying pressure
- Abdominal tenderness radiating to the umbilicus
- Pain in the abdominal area when legs are extended
Which of the following findings is NOT usually detected on the ultrasound scan of a gallbladder with cholelithiasis?
- Strawberry appearance of the wall of the gallbladder
- Gallstones
- Gallbladder wall thickening
- Edema of the gallbladder
- Dilated biliary tree
Which diagnostic procedure is performed when the position of the stone is inconclusive on a routine ultrasound scan?
- HIDA scan
- MRCP
- ERCP
- Repeat ultrasound scan
- X-ray
A 40-year-old woman had a minor accident, and an ultrasound scan was performed to rule out internal bleeding. Incidentally, the radiologist reported a 6-cm gallbladder stone. The patient is concerned. As her doctor, what will you tell the patient?
- "A cholecystectomy is done if a person is symptomatic."
- "Cholecystectomy cannot be done as an elective procedure."
- "Emergency cholecystectomy must be considered for your presentation."
- "Cholecystectomy is a futile procedure, and the stone will not cause any symptoms in the future."
- "Cholecystectomy is a risky and complicated procedure. However, I will perform it with ease on you."
Which of the following statements regarding cholelithiasis is NOT true?
- MRCP is the procedure of choice for decompression and sphincterotomy.
- Percutaneous drainage is done for acalculous cholecystitis.
- Cholecystectomy is avoided in patients who are asymptomatic.
- Elective cholecystectomy has a significantly lower complication rate.
- IV antibiotics and hydration are recommended for acute cholecystitis.
Customer reviews
3,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
1 |
Thank you very much for explaining this topic well. After a look through several youtube videos this was the best one!
1 customer review without text
1 user review without text