Playlist
Show Playlist
Hide Playlist
Fibromyalgia: Diagnosis and Management
-
Slides Fibromyalgia.pdf
-
Reference List Rheumatology.pdf
-
Download Lecture Overview
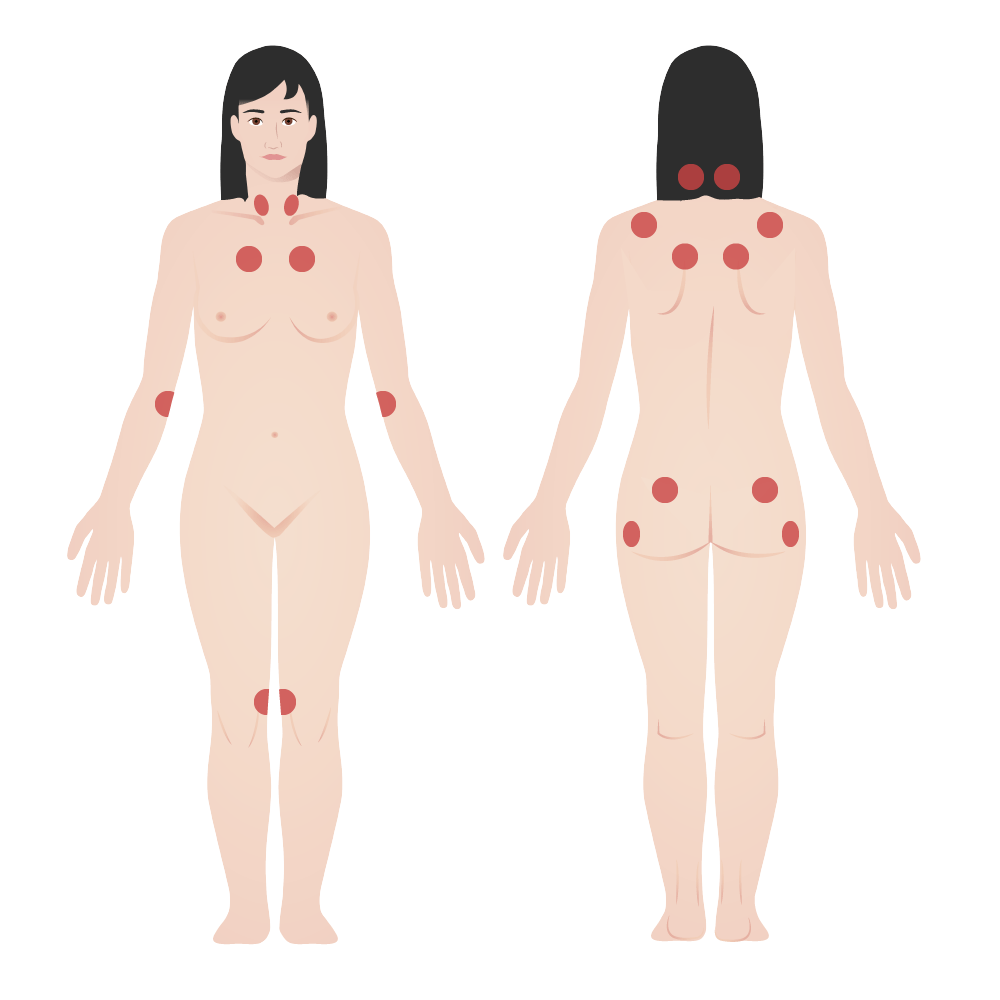
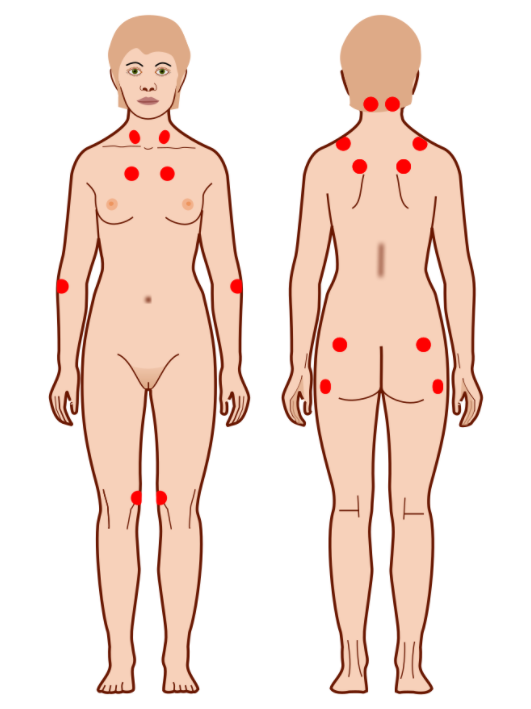
00:01 So let's talk more about what fibromyalgia is and in particular what the diagnostic testing is. 00:07 Now, we used to use these 18 trigger points shown here as the diagnostic test for fibromyalgia. 00:13 The clinician would basically push on those 18 areas and if more than 11 of them triggered pain and were particularly tender, we would say fibromyalgia. But there's increasing recognition over the past 5 or 10 years that this approach fail to incorporate these varied somatic complaints that patients experience. Patients basically oftentimes report fatigue, cognitive symptoms, waking unrefreshed, and a variety of other somatic complaints. And so the diagnostic criteria were changed to incorporate 2 main factors; the widespread pain index which is shown here which rather than the physician pushing on a bunch of locations, the patient subjectively reports where they're having different types of pain amongst these different colored areas and then secondly the symptoms severity score. This is a description of a constellation of different somatic complaints that patients may report and patients indicate again subjectively which of these symptoms they are experiencing. There are central type symptoms, cognitive ones, constitutional ones, then you've got muscular symptoms, joint involvement, urinary symptoms like she has been describing, don't forget about the eyes, joint of the jaw or the temporo-mandibular joint, issues with her chest wall, her stomach, and reproductive system as well. So the scoring system that we now use for fibromyalgia involves that widespread pain index and the symptom severity score. I know you'll note that when you look at all of those somatic symptoms that patients may report, you may see some overlap with some other non-inflammatory chronic pain syndromes. In addition to fibromyalgia, you may see patients report interstitial cystitis which our patient had. Tension headaches, myofascial pain syndrome which again is a localized or regionally associated sub-type of fibromyalgia, irritable bowel syndrome, temporo-mandibular disorders, and then chronic fatigue syndrome also known as myalgic encephalomyelitis. So fibromyalgia in these related conditions are all considered diseases of what's called centralized pain and that's in contrast with nociceptive pain. If you get punched in the arm, you'll have pain because of nociceptors in the cutaneous tissue there and neuropathic pain where a peripheral nerve itself is diseased or involved in some way. Centralized pain means that you won't find any evidence of inflammation on a tissue biopsy, instead the pathology in these conditions is believed to be a dysregulation in central processing of peripheral inputs leading to increased pain sensitivity. Complicating matters is the fact that many of these patients actually do have some other objective pain problem. For example, perhaps they have lupus or rheumatoid arthritis or some prior trauma that's believed to have likely set up this pain problem and primed the pain receptors such that they could develop centralized pain down the road. So let's talk about the management of fibromyalgia. First and foremost, it's about patient education. Patients oftentimes feel stigmatized because they've been to the emergency room multiple times for pain and nothing is ever found and they may feel dismissed by providers. 03:32 So you have to highlight to the patient that fibromyalgia is a real illness, it's characterized by the dysfunction of central integration of pain perception. It is benign, it's not life threatening, it's not disfiguring, and fortunately it tends not to progress. Patients should also be told that physical and emotional stress clearly exacerbates fibromyalgia and that needs to be a focus of treatment. You want your patients to increase their activity level, increase their sleep hygiene, and address any underlying mood disorders because we know that addressing those things will help to decrease their experience of pain. 04:06 When medications are necessary, particularly in the presence of comorbidities such as anxiety, depression, or primary sleep disorders, gabapentinoids like gabapentin and pregabalin may be prescribed. 04:17 Tricyclic antidepressants, most commonly amitriptyline, can be started at very low doses (5-10 mg at night). Other options, such as duloxetine or cyclobenzaprine, have also been shown to be beneficial. 04:29 Looking at the cognitive domain, cognitive behavioral therapy hands down very effective treatment for fibromyalgia without any accompanying side effects of course because it's not a medication and physical therapy is really important, getting these patients to be active rather than withdrawn and isolating. So, let's highlight a few key points. Fibromyalgia is a chronic, idiopathic, non-inflammatory, central pain syndrome characterized by diffuse musculoskeletal pain. It is a clinical diagnosis or a diagnosis of exclusion and again excluding the other diagnosis was fairly straight forward with an ANA, a TSH, and a CPK and some basic blood work. It is associated with neuropsychological and somatic complaints especially when patients report feeling foggy or having difficulty concentrating and the management is going to be multimodal, you're going to do physical therapy, maybe CBT, maybe medications and a real focus on education. There's our list of potential medications, sleep hygiene is important and as I said CBT.
About the Lecture
The lecture Fibromyalgia: Diagnosis and Management by Stephen Holt, MD, MS is from the course Miscellaneous Joint-related Disorders.
Included Quiz Questions
Which of the following is NOT considered a noninflammatory chronic pain syndrome?
- Polymyositis
- Fibromyalgia
- Interstitial cystitis
- Chronic fatigue syndrome
- Myofascial pain syndrome
Which of the following medications is most appropriate for the management of fibromyalgia?
- Pregabalin
- High-dose prednisone
- Hydrocodone
- NSAIDs
- DMARDs
What is the underlying cause of diffuse pain in fibromyalgia?
- Dysregulation of central pain pathways
- Peripheral neuropathy
- Tendon and muscle inflammation
- Autoimmune joint destruction
- Injury to peripheral nociceptors
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Clear diagnostic and management methods for FM. Well organized and easy to reference.