Playlist
Show Playlist
Hide Playlist
Fibroblast, Muscle Tissue & Synovial Cell Sarcoma
-
Rheumatology II 02 Synovial Cell Sarcoma.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
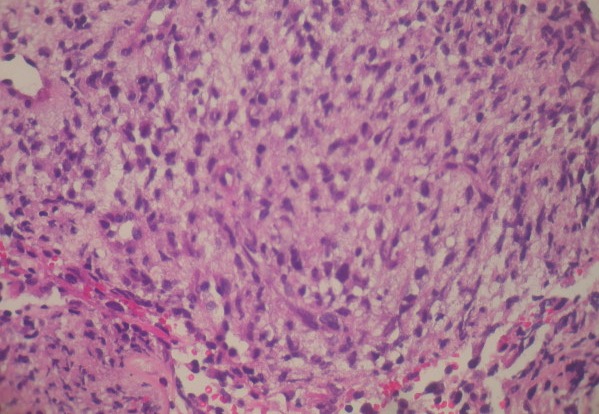
00:02 Here, our topic is fibro-. 00:05 We had a discussion of lipo-. 00:08 This is a discussion of fibro- under soft tissue diseases. 00:12 Under fibro-, in other words fibroblasts or fibrosis, is what you’re looking for. 00:18 Under this, we’ll divide this into superficial and deep. 00:21 At first, we’ll take a look at superficial. 00:24 Under superficial, poorly defined fascicles of mature-appearing fibroblasts surrounded by abundant amounts of collagen, of course, then giving rise to your fibrosis. 00:37 Now the 2 major places that you’re focusing upon with superficial fibromatoses would be the hand as you see in the picture and then the penis in a male. 00:46 Whenever there is fibrosis, in general, would you tell me as to what then happens to that particular structure? Good. 00:54 That would be contraction and often times there will be shrinking taking place, correct, of that organ. 01:00 Big examples there would include the liver undergoing cirrhosis and maybe perhaps the lung undergoing fibrosis. 01:07 With that said, if there’s fibrosis taking place here superficially of the hand, you’ll notice that the hand has now become flexed or the hand and then fingers become flexed like a claw, you then will call this Dupuytren palmer. 01:23 If the same kind of thing would then occur to the penis, then you would call this Peyronie’s disease. 01:28 P—penis, P—Peyronie. 01:31 Both of these are different locations of the same complication, known as superficial fibromatosis. 01:40 It will never, almost never metastasize, but it is locally aggressive, and often times, will recur even after excision. 01:52 You’ll notice here that, well this was supposed to be a bunch of fascicles of your muscle, but instead you see a sea, a sea of fibroblasts laying down collagen. 02:05 This is fibromatosis. 02:09 Whereas superficial fibromatosis was to the hand and to the penis, Dupuytren and Peyronie respectively, when you have fibromatosis taking place in the deep tissue, we now call this a Desmoid tumor. 02:24 D—desmoid, d—deep fibromatosis. 02:29 In terms of histology, it would be that of the same that you’ll find superficial, so lots of fibrosis. 02:35 The categories extra-abdominal, in other words, shoulder, chest wall, back, and thigh. 02:42 Extra-abdominal. 02:43 If it’s intra-abdominal, occur in the mesenteric or the pelvic walls. 02:48 And, if you’re thinking about familial adenomatosous polyposis, where the mutation taking place with APC and chromosome-5 and WNT, and all of the transcription factors, then here, with your deep fibromatosis, now we call this a variant of FAP, called Gardner syndrome. 03:12 Don’t forget that. 03:14 Once again, deep fibromatosis association with familial adenomatosous polyposis, is then called Gardner syndrome. 03:26 Continue discussion of fibroblast issues and soft tissue pathology. 03:30 Here we have fibrosarcoma. 03:32 So this is a malignancy, of course, once again composed of as the name applies, fibroblasts and collagen, middle age and elderly, deep tissue, and this particular type of pattern that you’ll find with fibrosarcoma is referred to as, by the textile industry— well they’re not the ones who actually did the histologic picture here— but I’m just saying, the name herringbone was adopted from the textile industry, and that’s the pattern you’d expect to find in fibrosarcoma. 04:05 Here we have rhabdomyosarcoma. 04:08 What does rhabdomyo- mean? Now we’re talking about skeletal muscle. 04:12 It’s a malignant tumor of a skeletal muscle. Rhabdomyosarcoma. 04:16 Here, you’re thinking about sarcoma taking place in childhood, and if it is— and I’ll talk about 2 different variants here in one second —but if it’s less than 20 years, then rhabdo- myosarcoma is what you have. 04:28 Usually, it will then occur at the head and neck or the GU tract, and look for the classic rhabdomyoblasts. 04:35 So once again, blasts then referring to premature cells. 04:39 If you then did have rhabdomyosarcoma in a young girl, let’s say for example, less than 5 years of age, and then way back in, well let’s say, female reproductive— let’s say that you’re looking at this girl’s genitals at 5 years of age, and you find with the naked eye, grapelike clusters coming out of the vagina. What do we call that? Good. 05:02 That’s called embryonal rhabdomyosarcoma, or in other words, you’ve heard of rhabdomyosarcoma. 05:08 You have your rhabdomyosarcoma or in other words called embryonal rhabdomyosarcoma in a girl perhaps less than 5 years of age— look for that grapelike cluster. 05:19 But in general, if rhabdomyosarcoma, less than 20 years, has nothing to do with embryonal rhabdomyosarcoma. 05:30 Here we will take a look at soft tissue pathology. 05:33 Unfortunately, quite common in population—young ladies, perhaps African American but could as well be Caucasian, maybe about 27 years of age, and then she complains that during her menses, she feels an awful lot of pain. 05:50 So in other words, we’re talking about fibroids or leiomyoma. 05:54 So during her menses, not only is she losing quite a bit of blood, but oh my goodness, she’s feeling dysmenorrhea. Right? Painful menses. 06:03 But what is leiomyoma? Leiomyoma is a smooth muscle benign tumor that is then occupying the space within or could be within the uterine cavity. 06:13 So you’ll call that intracavitary. 06:15 Or you could have a leiomyoma that’s located underneath the mucosa. 06:20 You then call that submucosal leiomyoma. 06:24 Or you could have one that’s located more in the periphery of the uterus by the serosa, and then you would then call that subserosal. 06:31 I bring those 3 locations of the uterine fibroma, or in other words, fibroids because each one of them gives you something different. 06:41 For example, if you find an intracavitary type of leiomyoma— if you actually take a look at the picture on the right here, see these polyp-like structures on the uterus? This is not a polyp. 06:52 These are well encapsulated smooth muscle whorled pattern which I will show you in description histologically of the leiomyoma. 07:01 Should have fewer than 10 mitoses per 10 hpf. 07:08 It’s benign. 07:09 What you’re looking at here a biopsy of leio- myoma would be that of whorled pattern. 07:13 So it’s one of those fibroids that we have taken the biopsy of it, and you find a whorled pattern of the smooth muscle cells. 07:25 This is leiomyosarcoma. 07:27 This is a malignant smooth muscle tumor, develops in skin and deep soft tissues of extremities and retroperitoneum. 07:36 Once again, here’s an example where a benign tumor such as a leiomyoma will not commonly give rise to a malignant smooth muscle tumor called leiomyosarcoma. 07:49 Pathology here would be painless, firm mass with malignant spindle cells with cigar-shaped nuclei arranged in interweaving fascicles. 08:03 A major issue within the synovium— it’s called synovial cell sarcoma. 08:08 So for example, in the picture here of x-ray of the knee and the joint capsule, and what you’re seeing there is increased opacity therefore represents the synovium undergoing massive proliferation, in which it has now become a sarcoma. A malignant tumor of your hinge joint. 08:28 For example, let it be the elbow, and in this case, the knee what have you. 08:32 Initially might have been thought of raised from your synovium. 08:37 Majority; however, will develop to large joints such as your knee and ankle, and you should think about adults. 08:44 Let’s take a look at the detailed pathology of synovial cell sarcoma. 08:50 Biphasic morphology of atypical spindle cells and the glands. 08:55 Well if you take a look at the picture here, a beautiful picture of your spindle cells, well if you see the vacuolated region there, and so is lined vacuolated region, are the glandular cells, alright? Now think of joint capsule. 09:11 Think of the synovial cells responsible for then secreting synovial fluid into your joint capsule, correct? So now let’s say you have a synovial cell sarcoma. 09:21 t only makes sense that you’d have a combination of spindle cells then surrounding your glandular cells that look like they’re about to secrete fluid into that structure. 09:33 Classic translocation that you must have committed to memory. 09:36 Translocation x-18 and a 5-year survival rate of 30% to 60%. 09:43 It’s quite variable. 09:45 This then now completes our soft tissue pathology section in which we then walk through the different organization, in other words, we looked at tumors of, let’s say, the smooth muscle, skeletal muscle, rhabdo-, and leio-. 10:00 We looked at issues of the lipid such as lipo- and here we finished it off by looking at issues in the joint such as synovial cell sarcoma.
About the Lecture
The lecture Fibroblast, Muscle Tissue & Synovial Cell Sarcoma by Carlo Raj, MD is from the course Muscle and Soft Tissue: Pathology. It contains the following chapters:
- Tumors in Fibroblast Tissue
- Tumors in Muscle Tissue
- Synovial Cell Sarcoma
Included Quiz Questions
The histologic finding of herringbone pattern is most characteristic of which of the following tumors?
- Fibrosarcoma
- Leiomyoma
- Rhabdomyoma
- Rhabdomyosarcoma
- Fibroma
A genitourinary tumor extending from the vagina in a 3-year-old girl that appears as "grape-like clusters" is most likely what type of tumor?
- Embryonal rhabdomyosarcoma
- Fibroma
- Fibrosarcoma
- Lipoma
- Liposarcoma
A 25-year-old woman is seen for menorrhagia, anemia, and infertility. Which of the following is a smooth muscle tumor that is most likely to cause these clinical manifestations?
- Leiomyoma
- Liposarcoma
- Rhabdomyoma
- Rhabdomyosarcoma
- Fibrosarcoma
A whorled pattern of smooth muscle cells is characteristic of what type of soft tissue tumor?
- Leiomyoma
- Leiomyosarcoma
- Rhabdomyoma
- Fibrosarcoma
- Fibroma
What type of tumor characteristically shows malignant spindle-shaped cells that have brightly eosinophilic cytoplasm and cigar-shaped nuclei?
- Leiomyosarcoma
- Leiomyoma
- Fibrosarcoma
- Fibroma
- Rhabdomyoma
Evaluation of a soft tissue mass around the knee in a young man reveals the chromosomal translocation t(X;18). What is the most likely diagnosis?
- Synovial cell sarcoma
- Rhabdomyosarcoma
- Fibrosarcoma
- Leiomyosarcoma
- Rhabdomyoma
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |