Playlist
Show Playlist
Hide Playlist
Female Pelvic Exam: Bimanual Examination
-
Reference List Physical Examination.pdf
-
Download Lecture Overview
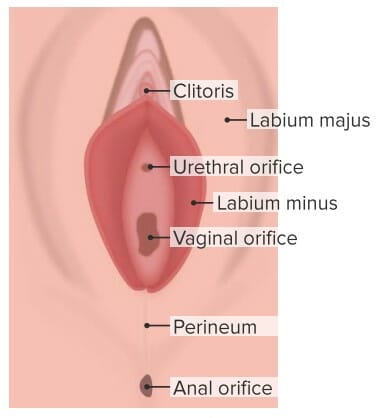
00:00 So before we move on to the genital exam itself, it's really important to maintain open lines of communication with your patient, this is a very sensitive exam. And especially if your patient has never had a pelvic exam performed in the past, you really want to make sure that your patient is aware of what's happening and what the specific sequence of events are going to be. So for the purposes of this session, we're going to pretend that our patient has never had this exam performed in the past. "So, my understanding is this is the first time you've had a pelvic exam and a Pap smear. Is that correct?" "Yes." "Okay." "So it's really important that we have an open line of communication. I want you to feel comfortable during this exam. You may need to have it again in the future so it's important that it is a fine experience for you. So, I'm going to preserve your modesty as best as I can throughout and only expose parts of your anatomy that need to be when I'm examining them and I'll also make sure that you're comfortable throughout." First off let me explain to you what the sequence of events is going to be. So, the first part is an external genital exam, just visually taking a look in the area then we're going to move on to an internal exam which is called the bimanual exam. "So I'm going to insert 2 fingers into your vagina and I'm going to be examining the cervix, examining the anterior and posterior wall of the vagina, etc."And then once we have completed that, I'm going to move on and use the speculum part of the exam. Now the speculum is here, I'm going to take this out of the bag now. So depending upon where one is having the exam performed, there are different types of specula that are out there. This is a typical disposable specula and importantly this is the bill of the specula and this is the part that's going to be inserted into your vagina. This is simply the handle and I'm going to have a light attached to it so you will see a black cable attached of the back here and that's in order to best visualize the cervix. So, that's the speculum or direct visualization part of the exam. In addition, when I performed that part of the exam, I want to be looking at the cervix so that I can collect cellular tissue. And so this is a Papanicolaou or Pap brush, and I'm basically going to be placing this right at the entrance of your cervix and spinning it several times in order to get cervical tissue that is then useful for screening for cervical cancer. Okay? And lastly, I have some other specimen tools here if in the event that we were concerned about a sexually transmitted infection I can swab for any discharge in the vagina and send it off for microbiology studies and similarly if I was concerned about trying to evaluate for a new vaginal discharge I can collect some of that discharge and then plate it out on a slide and do what's called either a wet mount or a KOH prep to try and figure out exactly what the cause of the change in vaginal discharge is. The last piece of equipment is actually a piece of equipment for you, and it's actually just this hand mirror. I found and it's been shown that it's useful for the patient to actually be able to see what is going on "because otherwise I'm on one end of the bed and you can't really see what's happening. 03:07 So you having some control being able to see the exam itself with a mirror is something that we encourage. So, I'll hand that to you once we're all set." Language, as you might imagine, is really important for this exam so you will note that I'm trying to avoid using overly clinical language like the word palpate which doesn't mean much to a lay audience, but I'm also trying to avoid words that can have particular connotations like I'm not going to use the word "I'm going to feel this area or touch this area." Instead, I'm going to use fairly neutral language like "I'm going to examine, I'm going to inspect, etc." "With that, I'm going to step out of the room and let you get into a gown and we will proceed with the exam." "Okay." "Okay, now that we've got your feet in this foot rest, I'm going to ask you now to simply just relax your legs and move them out to the side for me. Great. And we can _________ now. Okay?" "Great. You can hold that. Perfect." She's got her mirror in position so that she can see what we're doing. So now we are doing the external inspection of the pelvis and this starts off by first taking a look at the labia majora, also called the mons pubis area. There are different techniques here, but oftentimes you wanted to just use one hand to separate the labia so that you have one hand free, but for the purposes of this educational session I'm going to use both of my hands. Ideally you want to minimize contact with the patient's skin when you can, but in this case we'll use both hands. "So, you're going to feel me touching the outside of your vagina now." By doing that, I can now plainly see the labia minora on the inside there. Above it, we can see the clitoral hood and the clitoris. And then just inside the labia minora is the urethral orifice, right back there. "Pardon me. Can you relax your legs just a little bit more? Okay, great." And in this case, what I'm looking for is any evidence of any skin lesions, for example condyloma acuminata, evidence of a _____. Certainly a patient with candidal vulva vaginitis may have evidence of excoriations from scratching, a whitish discharge or some flaky scale on the outside of the vagina as well. And of course at this point I could also be looking to see if there is any excess discharge in the area. That essentially completes the external part of the exam, and so at this point we will go ahead and move in with doing the bimanual portion of the exam. So now we're going to proceed with the manual part of the exam and I'm just going to grab some lubricating gel here, and it's just for these 2 fingers. "And so, it's useful for you to take a deep breath and then breathe out and bear down as I'm inserting my fingers. And first off, I'm going to look actually on the outside of the vagina, looking specifically at the Bartholin's glands so you're first going to feel me separating the labia majora now. And relax your legs just a little bit. Great. And so now my finger is going to be inserted into your vagina. And just at the very bottom of the labia minora or the inside of the vagina is where I can feel the Bartholin's glands, which if somebody had a Bartholin's gland cyst that was inflamed that might be very painful or uncomfortable. And now, I'm going to insert my 2nd finger to the vagina, like so." And, what we'll do now is I'm just going to lift up. So with my hand up here, I can separate the lower folds here of the labia majora and I was going to ask you to bear down. Good. Relax. Good." And basically I'm looking for a rectocele to see if there is any bulging in of the rectum through the septum between the posterior vaginal wall to see if there is evidence of basically posterior vaginal prolapse. "And then by the same token, I'm going to push down and I'm now looking at the top of the vagina, the anterior wall. And go ahead and bear down for me again please. 07:31 Great." And I'm looking for any evidence of anterior wall prolapse or evidence of the vesicle, the bladder basically bulging in to the anterior vaginal wall. Having done that, I'm going to turn my hands over again. I'm just looking to inspect where the cervix is located. 07:48 And I found the cervix and that's going to help me later when I do my specula exam. "And I'm going to stand up and I'm going to basically inspect the size of your uterus. Okay?" "Uhuh." So using my left hand, I'm starting sort of by the umbilicus and I'm bringing my hand down slowly towards my fingers until I can feel the margins of the uterus. And since my fingers are on the cervix, I'll be able to feel as the uterus is shifted and I can feel that her uterus is appropriately positioned and not enlarged. And then likewise, I'm going to try and sweep her ovaries towards my fingers and my fingers now are on the lateral fornix around the cervix, which is to either side of the cervix is the lateral fornices. And I'm just trying to sweep her ovaries down towards my finger, which, as you might imagine you oftentimes cannot feel but in a particularly enlarged ovary you may feel it. Now I'm starting with the left ovary doing the same thing. My fingers are just in the lateral fornex and I'm trying to sweep her ovary down towards my fingers and I don't feel anything in this case. So "I'm going to withdraw my fingers now, and you can bring the sheet down again." That concludes the bimanual part of the exam. So now we'll move on to the speculum exam.
About the Lecture
The lecture Female Pelvic Exam: Bimanual Examination by Stephen Holt, MD, MS is from the course Examination of the Male and Female Genitourinary System.
Included Quiz Questions
What is one of the structures evaluated on the INSPECTION part of the female genitourinary exam?
- Labia majora
- Cervix
- Uterus
- Ovaries
- Bartholin's glands
What is one of the structures evaluated by PALPATION alone during a pelvic exam?
- Uterus
- Vulva
- Labia minora
- Clitoral hood
- Urethral orifice
What condition is the examiner looking for by elevating the anterior vaginal wall and inspecting the posterior vagina while asking the patient to bear down?
- Rectocele
- Cystocele
- Vaginal warts
- Lichen sclerosis
- Uterine prolapse
What organ is examined by using a speculum?
- Cervix
- Vulva
- Bartholin's glands
- Uterus
- Ovaries
What is the purpose of a Pap smear?
- To screen for cervical cancer
- To check for a tubal pregnancy
- To evaluate for ovarian cancer
- To screen for uterine cancer
- To screen for vulvar cancer
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
So great to see the real time exam! Very helpful.