Playlist
Show Playlist
Hide Playlist
Factors that Contribute to Coronary Atherosclerosis
-
Slides Ischemic Heart Disease.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
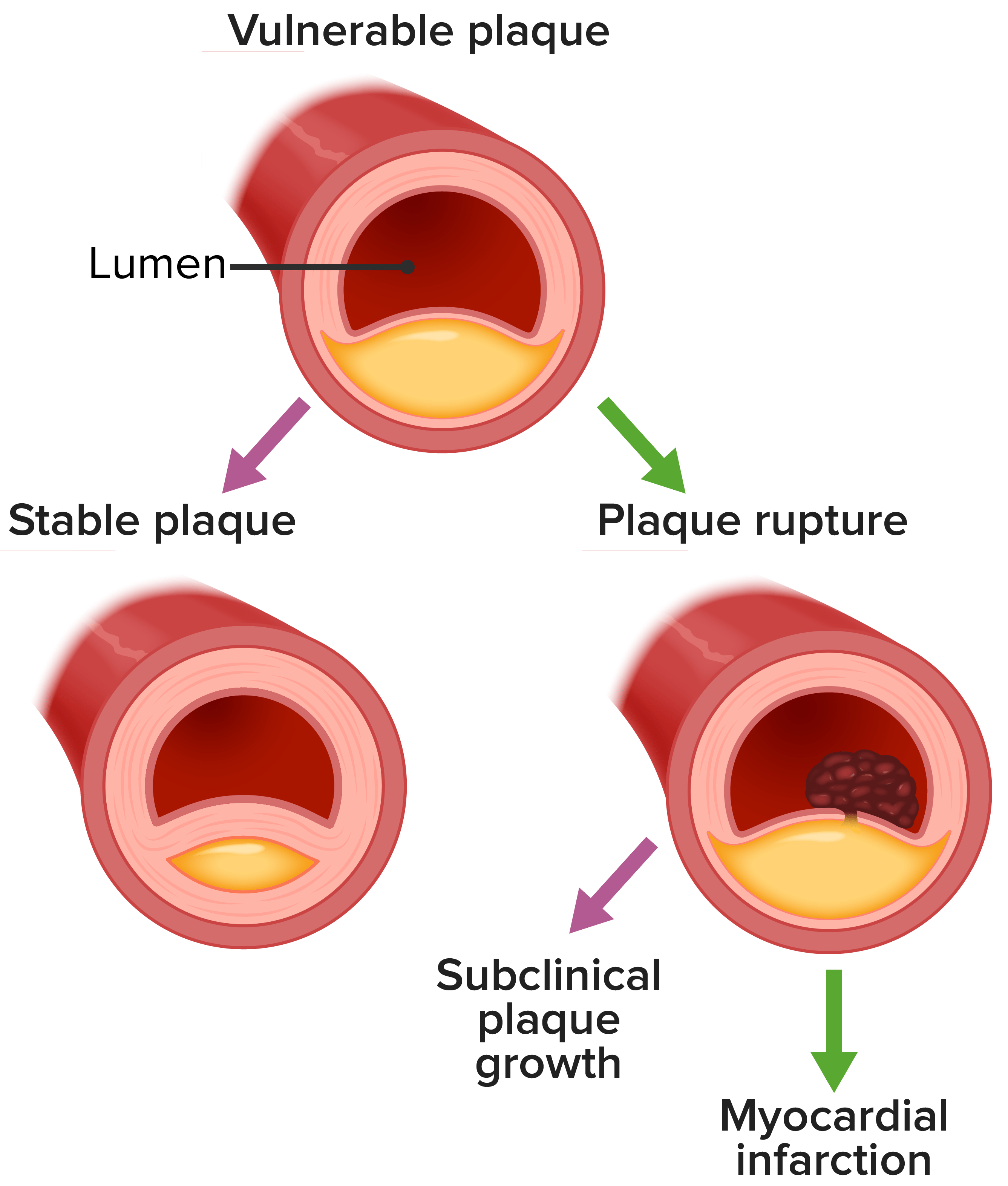
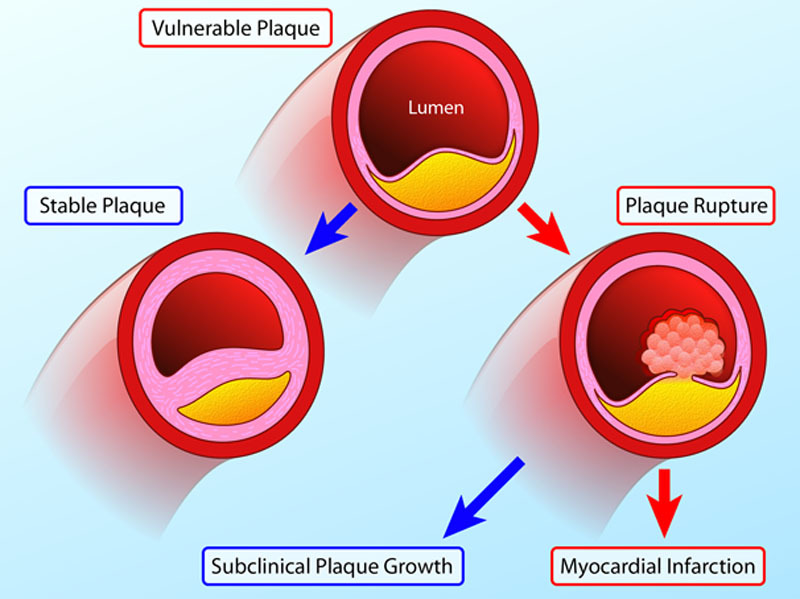
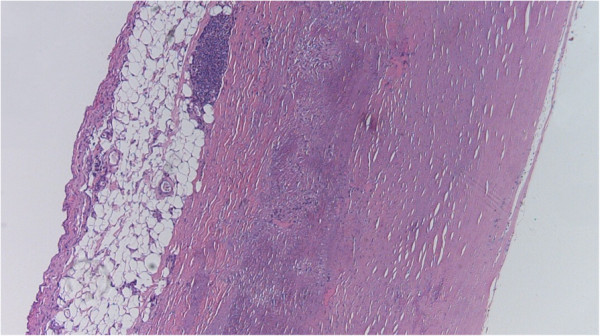
00:00 And as they say, there is a whole talk with me talking about mechanisms of atherosclerosis. 00:08 But in brief form, it's really primarily an inflammatory process. 00:14 It is driven by things like hypertension, hypercholesterolemia, diabetes, smoking, and genetics. 00:21 But basically, what we have are dysfunctional endothelial cells that then recruit inflammatory cells because they're dysfunctional. 00:31 They shouldn't do that normally but they do because they're dysfunctional for a variety of reasons. 00:35 And also, they tend to accumulate platelets. 00:38 The combination of those monocytes becoming macrophages and the inflammatory mediators they make and a combination of the platelets and the inflammatory mediators that those guys make, we end up with an atherosclerotic plaque. 00:50 And in there, we have lipids and cholesterol that have come through those dysfunctional endothelial cells. 00:56 And we have the recruitment of smooth muscle cells, primarily from the media, and we're going to form an atherosclerotic plaque formed of inflammation and smooth muscle cells and matrix and necrotic debris. 01:08 That gives us, potentially, a stable atherosclerotic plaque. 01:14 All atherosclerosis has a fibrous cap, a varying degree of smooth muscle cells, and the matrix they synthesize, and an underlying atheromatous core of necrotic debris, cholesterol, etc. 01:26 There's a smattering of inflammatory cells, and there's going to be angiogenesis. 01:31 Actually, remember, this is basically healing of an injured vessel wall which has a limited repertoire of things that it can do. 01:39 Okay, that's kind of a stable atherosclerotic plaque, but that plaque doesn't always remain stable. 01:45 And it doesn't always remain small. 01:47 So it can increase in size and compromise the vessel lumen which will cause ischemia, diminish blood flow or it can rupture suddenly, and then thrombose. 01:58 And those are the major complications associated with atherosclerotic disease. 02:02 So this is just showing you a coronary artery that had some degree of atherosclerosis within it, and that plaque ruptured. 02:10 We'll show you slides in a minute that will kind of highlight what this can look like. 02:15 But now, that rupture of the plaque suddenly will give a 100% degree of thrombosis, completely obstructing the vessel, and, now, no blood flow is going to the heart, and within 20 to 30 minutes, the heart muscle dies because it's not being perfused. 02:32 So that's the major acute cause of a myocardial infarct. 02:35 It doesn't always have to play out that way though. 02:38 And if you have significant atherosclerotic disease with diminished perfusion, you may have chronic low-grade ischemic injury to the myocytes. 02:45 So important take-home message that should scare you a little bit is that most plaque rupture occurs on a degree of stenosis that is not critical. 02:56 What do I mean by that? There's kind of a Rubicon. 02:59 There's kind of a limitation where if you have less than 70% chronic stenosis, then you have adequate blood supply to keep the heart happy and non-ischemic under most circumstances. 03:13 As soon as you have more than 70% stenosis, that's called critical stenosis, and little increases in your activity can precipitate angina. 03:22 Okay, so there's that 70% juncture for the most part. 03:26 That's when atherosclerosis becomes symptomatic at 70%. 03:30 But what I just said here on this bullet point is that most acute events that can cause fatal myocardial infarcts happen on lesions that are non-symptomatic. 03:40 They're less than 70%. So we can be walking around with a 30, 40, or 50% stenosis, be able to do things like run marathons and be totally asymptomatic. 03:51 And then one of those plaques, for various reasons that we'll discuss briefly in a moment, can rupture, and then we're dead. 03:59 So kind of building on that, partial occlusions can limit flow. 04:05 They can wax and wane and that can also potentially lead to unstable angina. 04:10 I'll explain the definition of unstable angina in just a minute. 04:13 But you can have changes when atherosclerotic plaque ruptures or erodes. 04:19 It doesn't necessarily have to be completely occlusive. 04:21 It can become partially occlusive in which case, you get symptoms that wax and wane. 04:26 So when we have partial thrombus, partial occlusion and partial thrombus because the plaque waxes and wanes, you can have thrombi. 04:37 Those thrombi actually produce potent activators of smooth muscle cell proliferation. 04:41 So they will augment. They will drive further atherosclerosis development. 04:46 Okay. That's a very brief, like, five slide description of atherosclerosis. 04:50 And I encourage you to go back and look at my other presentation on kind of more in depth discussion of why all this happens. 04:59 Okay. Things that contribute to coronary atherosclerosis and particularly plaque rupture is vasoconstriction. 05:06 So vasoconstriction by itself can compromise the luminal diameter. 05:13 And there are some forms of ischemic heart disease called Prinzmetal angina that happen just because the vessels focally constrict and limit flow. 05:25 But that change in vasoconstriction of a vessel can also increase shear forces and cause rupture of an atherosclerotic plaque. 05:38 Vasoconstricting factors include circulating adrenergic agonists, catechols. 05:43 So this is things like Epinephrine. 05:46 If you are shocked, scared, that can cause through the release of catecholamines, can cause a profound vasoconstriction. 05:57 There are locally released platelet contents that can cause vasoconstriction. 06:03 So, Thromboxane A2 released by locally activated and adhered platelets because we have a focal area of endothelial dysfunction can also cause vasoconstriction. 06:14 And then, the endothelium may be just dysfunctional. Not otherwise specified. 06:18 But normally, endothelium makes a variety of cell relaxing factors that will act on the smooth muscle cells and cause them to relax and therefore, dilate the vessels. That's nitric oxide. 06:28 Or they make contracting factors such as endothelin that causes the vessels to constrict. 06:33 So we can just have endothelial cells that are unhappy, whatever that means. 06:37 You can also have mediators that are released from perivascular inflammatory cells, monocytes, lymphocytes, even neutrophils that happen to be in the vessel wall can also profoundly impact the smooth muscle contraction or relaxation.
About the Lecture
The lecture Factors that Contribute to Coronary Atherosclerosis by Richard Mitchell, MD, PhD is from the course Ischemic Heart Disease.
Included Quiz Questions
What percentage of stenosis of the coronary artery is considered critical?
- 70%
- 10%
- 25%
- 50%
- 60%
Which of the following molecules causes vasoconstriction?
- Epinephrine
- Histamine
- Prostaglandin I2
- Bradykinin
- Nitric oxide (NO)
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |