Playlist
Show Playlist
Hide Playlist
Esophageal Carcinoma
-
Slides GIP Esophageal Carcinoma.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
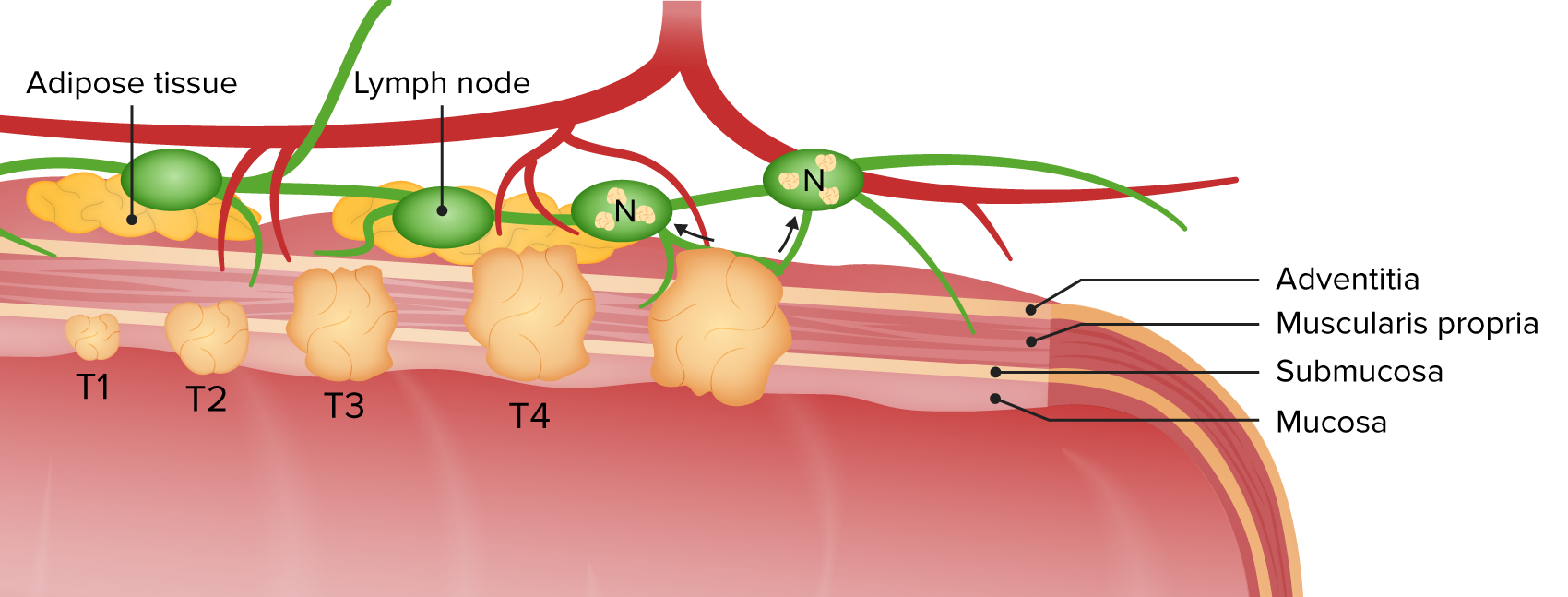
00:01 Welcome. In this talk, we're going to cover esophageal carcinoma, cancer of the esophagus. 00:06 Epidemiology. Overall, esophageal carcinoma is the 8th most common cancer worldwide and is also the sixth most common cause of all cancer-related deaths. 00:18 So this is not a good diagnosis for your patients to have. 00:22 The risk generally increases with age, especially in later years, in the sixth to seventh decade is when the typically peak occurs. 00:31 And for totally, not totally clear reasons, males are more affected than females. 00:39 So there are two varieties of cancer of the esophagus. 00:44 And it has to do with the kind of epithelial lining that is present. 00:49 So in a normal esophagus from top to bottom, it is lined by a stratified squamous non-keratinizing epithelium. 00:59 That's the normal situation. So the vast majority worldwide of esophageal cancers are going to be squamous cell carcinoma because that's the type of epithelial lining that's there. 01:12 And interestingly, about 90% of the esophageal cancers of the squamous cell carcinoma variety occur in what is indicated there, the esophageal cancer belt and this is potentially diet related or very high content of nitrosamines in the diet and that's usually what is implicated when we talk about the incidence in that location. 01:37 Now, in the US and in a lot of the developed parts of the world, the more common form of esophageal carcinoma is adenocarcinoma. 01:48 And you're thinking, "Well, how does an adenocarcinoma arise within a squamous epithelium? That's actually because recall with reflux of gastric acidity into the lower esophageal segment, we get a metaplasia. 02:02 We convert from a stratified squamous non-keratinizing epithelium to a more gastric or intestinal epithelium which is theoretically better able to deal with the gastric acidity. 02:14 That metaplasia now converts what is a stratified squamous epithelium to a glandular epithelium. 02:21 And so, because of the higher incidence of Barrett's metaplasia in these populations in the United States and developed parts of Europe, adenocarcinoma is the more common variety there. 02:35 The clinical presentation is largely what you might expect. 02:39 As we have an increasing mass that may ulcerate and bleed, you can have things related to loss of blood. You can have dysphagia, etc. 02:48 In the very early stages, patients will be entirely asymptomatic, may not even know that this is there. 02:55 There will however be, overtime, progressive dysphagia, difficulty swallowing and it progresses from something that is initially just dysphagia to solids to dysphagia for liquids. 03:08 And this is due to the expanding mass of tumor obstructing the lumen of the esophagus. 03:15 As we go further and further along with worsening dysphagia and then, tumor-associated anorexia, patients may experience severe weight loss. 03:25 And formally, pain or odynophagia will occur in about a fifth of the patients overall. 03:31 As you might expect, if there's bleeding, patients may actually have an iron-deficiency anemia. 03:36 Local tumor spread as the tumor expands or even metastasizes, will involve now local structures within the mediastinum. 03:47 So patients may have a cough related to tracheal invasion. 03:50 They may have hoarseness and vocal paralysis because of involvement of the recurrent laryngeal nerve. 03:56 They may actually, even as the tumor grows, it can invade and cause destruction and necrosis and you can form a tracheoesophageal fistula, so a direct connection between the esophagus which is more posterior and the trachea which is more anterior. 04:11 You can then have aspiration and other events related to the formation of that hole. 04:17 With metastatic disease, you can get compressive symptoms involving lymph nodes that can compress the aorta, that can involve the liver, lung, mediastinal structures. 04:29 Usually, when we think about metastatic disease, for squamous cell carcinoma, it's usually intrathoracic. 04:36 The tropism of the squamous cell carcinoma tends to be in that location. 04:41 Conversely, the adenocarcinomas typically have a tropism that is intraabdominal when they metastasize. 04:49 How do we make the diagnosis? A barium swallow study will typically show an asymmetric mirroring or a frank intraluminal masses. 04:58 If we do endoscopy, that actually allows us for direct visualization of a mass and a biopsy of lesions to confirm the diagnosis. 05:07 Very early legions may not look like very much. 05:09 It could be just kind of a superficial erosion. 05:12 With progressive time, they may become more nodular. 05:15 The overlying mucosa may ulcerate and there may be apparent irregularities around the base of the tumor. 05:23 With advancing lesions, you may actually see a near total obstruction of the lumen of the esophagus with strictures and etc. 05:33 So kind of a tabular form of thinking about these, the adenocarcinoma, more common in developed countries, typically involves the distal one-third of the esophagus where we're having reflux of gastric acidity, causing the Barrett's metaplasia. 05:46 And it's gonna be around the esophagogastric junction, EGJ. 05:50 Squamous cell carcinomas, more prevalent in that cancer belt, typically, across China. 05:58 It's the proximal two-thirds of the esophagus where we're going to have primarily, squamous cell epithelium. 06:05 The early lesions in adenocarcinoma will have mostly mucosal irregularities with ulceration, perhaps, a nodule. 06:12 And hopefully, in patients who have had chronic gastroesophageal reflux, we have been monitoring them for the development of Barrett's metaplasia. 06:23 And therefore, we may be able to pick it up relatively early because of our vigilance in surveilling them for a dysplastic change within the Barrett's. 06:33 On the other hand, squamous cell carcinomas early on may be quite subtle in appearance, but as they get larger and larger, they become quite brittle, variable. 06:43 They develop a lot of inflammation and new vascularization around the tumor with vascular or with mucosal erupt - or erosion and forming plaques and nodules. 06:55 And then, with advanced lesions in both cases, they tend to be very ulcerated, enlarging masses that protrude into the lumen. 07:04 And in the case of squamous cell carcinoma, they may go all the way around the esophagus, so called napkin ring-type lesions. 07:13 This is just showing you typical findings on histology. 07:16 So this is what I do in my day-to-day life in terms of diagnosing biopsies that come out. 07:23 And we'll do a biopsy of the mass and you can see on the left-hand side, normal, stratified squamous epithelium. And then, you see the tumor. 07:30 Itís brown because we've used a specific stain to identify intracellular keratin but you can see that there are clearly dysplastic elements that are invading deep within to the submucosa. 07:43 The adenocarcinoma on the right-hand side, I'm not showing you any normal mucosa there. 07:48 That's completely all tumor forming kind of nascent glands, ill-defined glands. 07:55 Management. So this is cancer. We already know that this has a very bad prognosis overall. 08:01 So what do we try to do? Well, we try to find it as early as possible. 08:05 Once we identify it, we try to resect it. 08:07 If we happen to catch it early for any of a variety of reasons and there's limited size, we can actually do it as an endoscopic procedure. 08:15 That tends to be the minority of cases. 08:19 And in the vast majority of circumstances, we're gonna have to go to open surgery. 08:23 So we'll do an esophagectomy. We will remove that portion of the esophagus and associated draining lymph nodes. 08:30 We will reanastomose what's left of the esophagus, often with a pull up of this gastric epithelium and portions of the stomach. 08:39 And then, we reanastomose that so the patient can have normal swallowing and movement of food from top to bottom. 08:45 If we have to do esophagectomy, we often will do neoadjuvant therapy which means we anticipate that there;s going to be metastatic spread. 08:53 And so we will give the patient chemotherapy, usually, in advance. 08:57 And then, follow-up chemotherapy. 09:00 If the patient is diagnosed with metastatic disease at the beginning, it may not make sense to do an open-procedure and put them through all of the morbidity associated with surgery. 09:13 And so we may do palliative options. 09:15 So to allow food to go from top to bottom, we'll put in a stent but weíre not gonna resect the tumor. The prognosis. 09:23 So it all depends at what stage that we catch the tumor at. 09:27 And unfortunately, the majority, greater than 50% and up to 80% of patients, on initial presentation where we make our first diagnosis, they have locally advanced or metastatic esophageal cancer. 09:43 And so this is showing you the five-year survival rates. 09:45 If you have stage one disease, cancer restricted just to the esophagus, no local invasion into other structures, no nodal metastasis, your five-year survival is about 50%. Not great, not terrible, but just not great. 10:02 If you have locally invasive tumor, with or without nodal involvement, so that is stage two disease. 10:09 Your five - your five-year survival goes down to about 25% and if at the initial presentation, the initial diagnosis, you have distant metastasis documented by liver mets or more distal nodal metastasis, not local, but distal, than your survival is miserable at about 5%. 10:30 We can have also biomarkers that give us a rough idea of prognosis as well. 10:35 And in particular, it turns out that the tyrosine kinase, the HER2 receptor, overexpression of that is associated with a very aggressive course and overall, very poor survival even if you catch it at a stage-one disease. 10:51 So not be a bummer about this but esophageal cancer, bad actor and hopefully, none of you will ever experience it. With that, we'll close.
About the Lecture
The lecture Esophageal Carcinoma by Richard Mitchell, MD, PhD is from the course Disorders of the Esophagus.
Included Quiz Questions
What is the most common type of esophageal carcinoma worldwide?
- Squamous cell carcinoma
- Adenocarcinoma
- Basal cell carcinoma
- Gastrointestinal stromal tumor
- Goblet cell cancer
Which type of esophageal carcinoma is associated with Barrett metaplasia?
- Adenocarcinoma
- Squamous cell carcinoma
- Gastrointestional stromal tumor
- Basal cell carcinoma
- Goblet cell cancer
What is NOT a typical symptom of esophageal cancer?
- Diplopia
- Weight loss
- Dysphagia
- Anemia
- Cough
What is needed to diagnose esophageal adenocarcinoma?
- Biopsy
- CT neck
- Modified barium swallow
- PET/CT
- Chest X-ray
What is the five-year survival rate for esophageal cancer limited to the esophagus?
- 50%
- 25%
- 15%
- 85%
- 35%
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
This is a very important topic in my country (Guatemala), thank you Dr Richard.