Playlist
Show Playlist
Hide Playlist
Erythema Nodosum: Pathophysiology
-
Reference List Pathology.pdf
-
Slides Erythema Nodosum Pathophysiology Dermatopathology.pdf
-
Download Lecture Overview
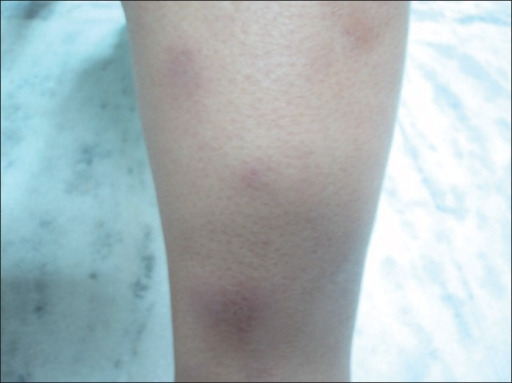
00:01 Welcome. In this talk, we're going to discuss one of the very most common forms of panniculitis, that is to say erythema nodosum. 00:10 For a general overview of panniculitis, I refer you back to one of the other talks that's in this series. 00:16 And we were a little vague about the mechanisms overall, but in this case, we'll get right down and dirty and get into this. 00:24 So erythema nodosum is an immune mediated form of panniculitis. 00:28 So that's inflammation of the subcutaneous fat. 00:30 And it is fundamentally a very good example of a type four hypersensitivity reaction. 00:37 Elsewhere in the collection of Lecturio files you will find a really good discussion on type four hypersensitivity reactions. 00:46 I'd say it's excellent because I did them. 00:49 Okay, so let's do the epidemiology of specifically erythema nodosum. It typically is in women in the second to fourth decades. And again most autoimmune diseases are more common in women than in men. 01:03 Uh, all ages and all racial groups are represented. 01:06 And as I already alluded to, it is the most common form of panniculitis. The pathophysiology of this. 01:14 So although we know it's a type four hypersensitivity response, we really don't entirely understand the driving triggering mechanisms in about half of cases. In the other half what is driving it appears to be an infection. And typically this is a streptococcus infection. 01:31 So a skin infection. It's curious though because the predilection, the actual classic manifestations involve just the lower legs over the shin and the calves. 01:42 And yet the streptococcus would be present pretty much all over the skin. 01:46 Theoretically in the individual's microbiome. 01:49 So why the legs? We don't really know. 01:53 Other agents that can cause erythema nodosum are oral contraceptives. And notably pregnancy may be a driver for this. So estrogen levels, estrogen spikes may be important in driving the process. Penicillin, sulfonamides, other drugs are associated with it. 02:12 Other autoimmune diseases like inflammatory bowel disease, may be a driver for erythema nodosum. 02:19 Malignancy, particularly hematologic malignancies, and some of the carcinomas may be a reason. 02:25 And if everything else is ruled out in terms of an etiology and you're trying to find something, perhaps an occult malignancy is lurking someplace. 02:34 And then, as I've already mentioned, pregnancy can be an initial driver and sarcoid, which is another inflammatory autoimmune disease. 02:42 So the classic pathway for all of this is a type four hypersensitivity response. Some sort of initial stimulus, whether it's tissue damage or an infection, elicits a type one CD4 T cell-mediated response. 03:00 This is just the typical response to other injury within the body that CD4 type one Th-1 response is then going to recruit and activate secondary effector cells, including macrophages and neutrophils. 03:21 So depending on the kind of differentiation of the initial CD4 response, we may get cells that are predominantly Th1 driven making interferon gamma which is going to stimulate macrophages or and or they may be Th-17 differentiated in which case they're going to make a lot of IL-17 and IL-22 and 23 that are going to be responsible for recruiting neutrophils. 03:49 A combination of the activated macrophages and neutrophils in the area that is being responded to will cause vascular injury, will cause tissue injury, and will lead to the manifestations that we recognize as erythema nodosum. 04:05 The clinical manifestations of this because we are eliciting an immune response, there may be prodromal symptoms before we see the actual cutaneous or subcutaneous lesions on the skin. 04:16 That prodromal symptom constellation will include fatigue, fever, malaise, arthralgia, and arthritis. 04:24 You're seeing the effects of of interleukins on the body more systemically. 04:28 The classic skin lesions we've already seen when we were discussing previously panniculitis. But I will repeat them here. 04:37 You have erythematous red tender nodules on both shins. 04:42 They tend to be non-ulcerated . 04:43 So we've not typically caused ischemic necrosis of the overlying epidermis although that can happen. 04:49 They tend to be fixed somewhat in the skin. 04:52 There's a lot of inflammation and fibrosis involving the deep fat. 04:56 So it tends not to be something that feels particularly mobile. 04:59 They are slightly raised because of the induration, the edema, and the inflammatory cell infiltrate. 05:04 They can range in size anywhere from a couple centimeters all the way up to five centimeters. Um, the lesions will come in crops and develop over several years. Um, they're usually self-resolving with time in the particular location where you have this inflammatory response. 05:23 You will also have a secondary regulatory T-cell response. 05:27 And within a couple within a couple of months overall we'll see resolution of the original lesions. But there may be some residual bruising with deposition of hemosiderin or residual hyperpigmentation related to focal hypermelanin production that will occur and may persist following resolution. Although the most common site is over the lower limb and particularly over the shin and calf. 05:53 Ankles, thighs, buttocks, calves, and face can also be places where this occurs. How do we make the diagnosis? Well, in fact, a large part of this is clinical. 06:04 It's the right-looking disorder in the right location, on the right patient with the right story. 06:11 But you can also do laboratory studies to help nail down the diagnosis. A CBC is going to be important for making sure we don't have some sort of underlying hematogenous malignancy or, and, or an ongoing infection. 06:28 Uh, erythrocyte sedimentation rate or C-reactive protein are going to be good kind of markers for the inflammatory status of the individual. 06:36 Throat culture and antistreptolysin -O may help us to nail down whether streptococcus is in the mix as a cause for this particular patient's erythema nodosum. You might want to do a tuberculin skin test, and look for the possibility that this does represent some other, more insidious organisms, such as Mycobacterium, and then finally a pregnancy test. 07:01 Remember that I told you that elevated estrogens. 07:06 Birth control pills and or pregnancy can be a trigger for erythema nodosum. Clearly, if you're dealing with a postmenopausal woman, that's not going to be the case, but a 30-year-old with such lesions, you will look like a genius by having also remembered to do a pregnancy test. 07:24 How do we manage this? Well, in fact, it's usually self-limiting and usually will resolve within a couple of months. But there may be recurrent crops of lesions. 07:34 And so you want to kind of prevent that. 07:37 So the underlying cause should always be attempted to be identified. And then we can go after that. 07:44 So if there's an infection then we want to treat that appropriately with antibiotics. Symptomatic treatment for the lesions themselves, rest, leg elevation, venous compression stockings, analgesics, and if we can rule out an infectious cause then give systemic corticosteroids and the patient will feel better but there will also be much less inflammation. 08:08 And with that, the most common cause of panniculitis, erythema nodosum.
About the Lecture
The lecture Erythema Nodosum: Pathophysiology by Richard Mitchell, MD, PhD is from the course Inflammatory Lesions of the Skin.
Included Quiz Questions
Which population is most commonly affected by erythema nodosum?
- Women in their 20s-40s
- Men in their 50s-70s
- Children under 10 years
- Women in their 60s-80s
- Men in their 20s-40s
What is the most common infectious trigger of erythema nodosum?
- Streptococcus
- Tuberculosis
- HIV
- Candida
- Staphylococcus
Which area is most characteristically affected by erythema nodosum?
- Shins and calves
- Face and neck
- Upper arms
- Chest and back
- Hands and feet
Which initial test is most appropriate for evaluating suspected erythema nodosum in a 30-year-old woman?
- Pregnancy test
- Skin biopsy
- Genetic testing
- Allergy testing
- Vitamin D level
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |