Playlist
Show Playlist
Hide Playlist
Erythema Multiforme: Pathophysiology
-
Reference List Pathology.pdf
-
Slides Erythema Multiforme Pathophysiology Dermatopathology.pdf
-
Download Lecture Overview
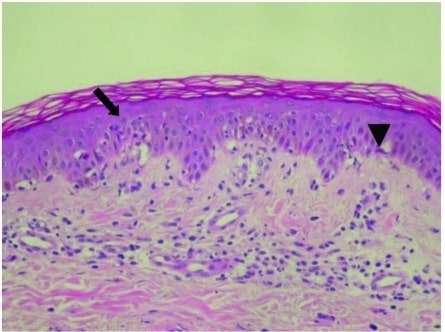
00:01 Welcome. The topic for this talk is erythema multiforme, which is a very interesting lesion with a very characteristic rash. 00:10 So erythema multiforme or EM is a targetoid lesion. 00:16 And this is not named after a certain department store chain in the United States, but rather is based on the fact that it looks like a big bullseye. 00:25 And there may or may not be systemic symptoms, but the characteristic lesions are what kind of give this this entity its particular designation. 00:35 The epidemiology of this is it's not all that common. 00:39 So a global incidence of maybe 2 million cases annually, given that there are 7 billion people or so on the planet, it's kind of 1 in 2000. 00:48 So not that common, but you will encounter it probably at some point or another in your careers. It is more common in young adults, typically less than 30 years of age, men greater than women, for reasons that are not clear to me. 01:01 And maybe one of you out there has a better idea. 01:04 So with regard to pathophysiology, the vast majority of cases of erythema multiforme, 90% or more are going to be infectious. 01:14 Leading the charge is going to be viral infections and in particular those associated with herpes simplex virus type 1 or 2. 01:22 They are going to be maybe up to 50% of all the causes of erythema multiforme. So keep that in mind. 01:29 Epstein-barr virus can do this and certainly other viruses as well. 01:33 In other categories bacterial infections. 01:35 And you see a list there of potential bacterial infections can also be a cause for erythema multiforme. 01:44 Similar targetoid lesions also occur in Lyme disease. 01:48 Borrelia infections, which are more common, as you're probably aware, in the northeastern United States. 01:54 On clinical grounds alone, you can't really distinguish erythema multiforme versus the targetoid lesion that occurs with Lyme disease, although the Lyme disease tends to be single lesions and erythema multiforme tend to be multiple lesions. 02:11 But on clinical grounds can't tell them apart, and you need to keep that in your differential as well with target lesions. 02:19 Fungal causes can also be involved with erythema multiforme, although typically less frequently. 02:26 Of the noninfectious causes, we have three general categories, and one is going to be drugs. 02:31 And there's a panoply of drugs that can be associated with erythema multiforme. 02:37 Secondly, malignancy occult malignancies, particularly leukemias and lymphomas are certainly a possibility. 02:44 And if you rule out everything else that rises to the top of your differential. 02:49 And then finally, a variety of autoimmune diseases, inflammatory diseases not otherwise specified, including sarcoid, lupus, polyarteritis nodosa that lead to kind of a systemic pro-inflammatory state that can also manifest with the targetoid lesions that we see in erythema multiforme. 03:08 Erythema multiforme is characterized or classified as either minor or major based on the presence or absence of one, mucosal lesions, two, systemic symptoms. 03:18 So systemic symptoms would be fever, night sweats, weight loss, joint and muscle aches and pains, that sort of thing. If you just have the rash it's a erythema multiforme minor. Add the other ones on top and now you're into major category. 03:34 What's going on? So remember I said HSV was the most common infectious cause about 50% of the cases. And what is happening is that the the keratinocytes are infected with HSV. HSV is now driving the production of various antigens, various viral proteins that can be expressed and then subsequently recognized on the surface of the keratinocytes. 04:00 And then you have HSV-specific helper T cells, typically of a Th1 phenotype. 04:06 So they're going to be driving the production of certain pro-inflammatory cytokines such as interferon gamma. The upregulation of those pro-inflammatory cytokines and chemokines drives the subsequent recruitment of inflammatory cells, NK cells, CD8 cells, other additional CD4 positive T cells, and macrophages that will then in turn cause keratinocyte damage via all those mechanisms. 04:33 So we have kind of a infection recognized by host, recruitment of inflammatory cells and then damage to the infected cells. 04:44 And that's how we're getting the targetoid lesions of erythema multiforme. 04:49 The clinical presentation. 04:50 Well again like most things in dermatology or dermatopathology it's by inspection. So it will be, the lesions will typically begin as erythematous that is to say red flat macules that over 3 to 5 days as we recruit more inflammatory cells convert into papules and eventually the targetoid lesions. 05:12 And these are typically 1 to Three centimeters in diameter, so they're pretty big and not easy to miss provided you actually look for them. They tend to be symmetrical and a peripheral distribution on extensor surfaces. 05:28 So kind of like that. And like that there's a centripetal spread. 05:32 So they start trunk and then they go out to the periphery and they tend to be quite itchy or pruritic. The mucosal lesions are very painful. 05:42 They are erosions and ulcers within the mouth and on the lips. 05:47 You can also get involvement around the eyes so the ocular mucosa and then the genital mucosa and anus. They usually erythema multiforme, as the immune system responds and then we get the counter-regulatory mechanisms. 06:01 We typically get spontaneous resolution within about a month. 06:04 And there are no long term sequelae, although the lesions can recur because again if infection is a major driving force, if you get reinfected, yes, you can go through that cycle again entirely. 06:17 How are we going to diagnose this? Well, it's the clinical presentation. 06:22 It's how they look. We can also, since we know that 90% of these are going to be due to some infectious entity, we can do serologic testing to try to identify that in patients who also have respiratory symptoms, you want to look for certain mycobacteria. 06:36 But in patients who have and the most common one being HSV herpes simplex virus, you want to look for that and particularly if it's recurrent, that tends to be the major player in recurrent erythema multiforme. 06:51 The biopsy somewhat nonspecific. 06:54 A lot of things look like this. 06:56 So it's the biopsy per se is not going to nail the diagnosis. 06:59 But it will rule out some other things. 07:02 And what you're going to see is damage to the epithelium. 07:05 And that's represented as kind of vacuolated and degenerated keratinocytes at the Dermoepidermal junction. 07:12 You're also going to see some dermal inflammatory infiltrate mononuclear cells. You may also see vascular congestion vascular dilation as well as edema within the dermis, but again somewhat of a nonspecific picture. How do we manage it? Well, as I said before, it's mostly self-limiting and doesn't typically require treatment. 07:35 However, if there's recurrent disease, we may want to consider getting rid of the causative agent, particularly infectious agents. 07:44 Symptomatic therapy. When it's really itchy or involves the mouth, we can give topical corticosteroids or oral antihistamines to kind of lessen those itchiness. And then we can give anesthetic mouthwash for oral lesions and for recurrent erythema multiforme that you get over and over and over again. 08:05 You may want to give continuous acyclovir therapy for the virus for six months as a suppressive therapy. 08:13 With that covered we targeted a very characteristic lesion and talked about it from beginning to end. 08:20 Thanks.
About the Lecture
The lecture Erythema Multiforme: Pathophysiology by Richard Mitchell, MD, PhD is from the course Inflammatory Lesions of the Skin.
Included Quiz Questions
What is the most common infectious cause of erythema multiforme?
- Herpes simplex virus
- Epstein-Barr virus
- Mycobacterium
- Borrelia burgdorferi
- Streptococcus
What feature distinguishes erythema multiforme major from minor?
- Presence of mucosal lesions and systemic symptoms
- Size of skin lesions
- Number of targetoid lesions
- Duration of symptoms
- Distribution pattern
How do the skin lesions of erythema multiforme typically evolve?
- Red macules to papules to targetoid lesions
- Papules to vesicles to ulcers
- Vesicles to bullae to scars
- Targetoid lesions to macules to papules
- Pustules to crusts to scars
Which treatment is most appropriate for recurrent HSV-induced erythema multiforme?
- Six months of suppressive acyclovir
- Topical steroids only
- Oral antihistamines only
- Antibiotics
- Systemic steroids
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |