Playlist
Show Playlist
Hide Playlist
Ectopic Pregnancy: Diagnosis
-
Emergency Medicine Bord Ectopic Pregnancy.pdf
-
Download Lecture Overview
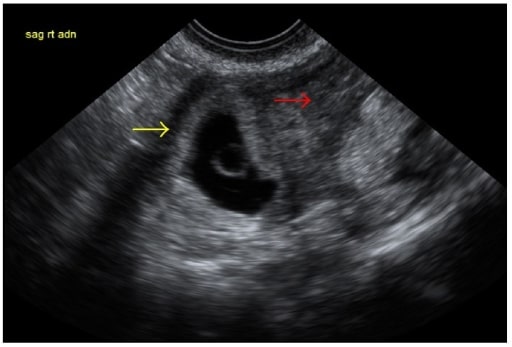
00:02 The other big diagnostic tool for ectopic pregnancy is checking a serum HCG. 00:07 HCG is a hormone secreted from the growing fetus. 00:12 And in the first 6-7 weeks of pregnancy the beta HCG will double every 1.8 to 3 days. 00:19 So you can follow serial levels. 00:21 In the Emergency Department on that first visit, you’re just gonna be able to get one discreet level but there's a following of serial level, so following levels for patients if they're discharged or even if they have an ectopic pregnancy that’s treated can be very helpful. 00:36 Because you want to see in a normal pregnancy, those levels will double that every 1.8 to 3 days, but in an abnormal pregnancy like an ectopic pregnancy, those levels will not be doubling, those levels will be going down. 00:52 So what does the HCG level tell you about what you should see on your ultrasound? So for normal intrauterine pregnancy, that’s a pregnancy that’s implanted in the right place that’s developing normally. 01:16 On a transvaginal ultrasound, you would start to see stuff at a levels 1000-2000. 01:23 However, ectopic pregnancy has been diagnosed at very low levels of HCG. 01:28 So what is this telling us is that we don’t wanna go ahead and use our HCG levels to talk us out of getting an ultrasound or to tell us not to get an ultrasound or for us to call our radiologist to say, "Well, the HCG is 500, we’re not gonna get an ultrasound." Ectopic pregnancy can be diagnosed at very low levels. 01:48 It will help you interpret what you see the HCG. 01:51 But it won’t necessarily or should never talk you out of getting a test. 01:55 I personally have diagnosed ectopic pregnancy in a patient who had an HCG level of 250. 02:01 And I know people who have anecdotally had ectopic pregnancies diagnosed with levels in that range. 02:08 So go ahead and check the level, but don’t let it use you. 02:12 Don’t use it to talk you out of getting the test. 02:16 What other blood work should you get for your patients? So you’re working on getting an ultrasound, you’ve checked the HCG level. 02:22 You want to check the CBC. 02:24 Now even in ruptured ectopic pregnancy, the hemoglobin may be normal. 02:28 And the reason for that is that it takes our body sometimes a little bit to equilibrate, and have that hemoglobin have her reflect and have it dropped and have them be a reflection of the bleeding. 02:39 The other very important lab to send is the type and screen. 02:42 And the reason that we send the type and screen for all patients with vaginal bleeding in pregnancy is to prevent the blood type from the mother reacting with the blood type from the baby. 02:53 So if someone has a negative blood type, so if they’re A negative, O negative, that patient will need RhoGam. 02:59 And the reason we give RhoGam is we use it to prevent future Rh incompatibility. 03:05 Because the issue would be, if the baby had positive blood, so the fetus that’s developing has positive blood and the mother has negative blood and those blood types get exposed to one another. 03:17 They can react to one another. 03:19 And then the mom can make antibodies to that blood type and if she were to get pregnant again, then that will cause issues with future pregnancy. 03:29 You know, if you’re concerned that the patient will need surgery or a blood transfusion, a type and cross maybe beneficial. 03:35 So type and screen tells you the blood type and whether the patient has a negative or a positive blood type. 03:40 Type and cross is when you start getting blood ready for the patient. 03:44 So that’s when you start preparing the blood. 03:48 Now the ultrasound is your test of choice and your imaging modality of choice to diagnose it. 03:53 Ultrasound will show an ectopic pregnancy either in the fallopian tube or within the corner of the uterus. 04:00 And basically, it will look like a gestational sac or a very early developing fetus in that area. 04:06 Sometimes, depending on how far the pregnancy is advanced, you’ll see fetal heart tones as well. 04:14 You know, this ultrasound is actually an example of an indeterminant ultrasound. 04:18 So what happens with some people who present vaginal bleeding in early pregnancy is you’ll get the ultrasound and the ultrasound will show an empty uterus. 04:28 It won’t show anything in the uterus. 04:29 It won’t show a normal intrauterine pregnancy, but it also doesn’t show an ectopic pregnancy. 04:35 So we want to be thinking about what we’re gonna do for these patients and how we're going to advise them because we don’t have a clear diagnosis right now. 04:43 So if your ultrasound is indeterminant, so what we mean by that is you do the ultrasound and you don’t see an ectopic pregnancy and you don’t see something in the uterus. 04:52 Ectopic pregnancy is more likely if the HCG levels are less than 1000. 04:57 You know, if your HCG levels are above 1000 or above that discriminatory zone at 1000-2000 range, you might be starting to wonder where the pregnancy in fact is. 05:08 In those situations, you may need to consult ObGyn to help them sort out what the next best steps are for that patient. 05:16 Now, if your patient is unstable or there’s evidence of irritation to the peritoneal cavity, so their belly is tense and rigid, they have a lot of guarding or rebound tenderness, the next step here should be a point of care ultrasound FAST in the ED to look for free fluid. 05:35 So what that is, the FAST scan is discussed in other lectures on trauma. 05:39 But what it looks for is it looks for free fluid in the abdomen. 05:43 So if someone has a ruptured ectopic pregnancy, they're going to have blood in their abdomen. 05:49 So that point of care ultrasound FAST can do a good job at looking and seeing if there's any blood in the abdominal cavity. 05:57 Now again, if you see blood in the abdominal cavity and that patient has a positive pregnancy test and they’re unstable, you get on the phone and you get your patient to the operating room as quickly as possible. 06:09 You know, if the work up is unrevealing, so let’s say, you’re not really sure what’s going on. 06:13 The ultrasound isn’t very revealing, the patient's lab values aren’t super revealing, but your patient is unstable, so they still are hypotensive, they’re tachycardic. 06:23 That patient may benefit from a diagnostic laparoscopy. 06:27 So what basically happens there is the OBGyn team goes in to the abdomen and they take a look. 06:33 And they see if there’s any evidence of bleeding or any concerns that weren’t seen necessarily on the other imaging studies. 06:42 Laparoscopy is the surgery that takes place using the cameras. 06:46 So the patient won’t have a big open scar or anything along those lines in case something isn’t found. 06:52 Beware of the heterotopic pregnancy. 06:55 So heterotopic pregnancy, what that means is it means that you have one pregnancy that’s implanted in the uterus, so one intrauterine pregnancy and one ectopic pregnancy. 07:07 So the patient essentially has two pregnancies in the body. 07:10 One being normal and one being implanted in an abnormal place. 07:14 You know, this is relatively rare in spontaneous conceptions. 07:18 I actually have taken care of one individual in my life that's had this via a spontaneous conception. 07:24 But there's increased incidents of this in patients who are undergoing in-vitro fertilization. 07:31 Always make sure that you’re thinking about this. 07:32 This is another one of those reasons that I go ahead and I get formal ultrasounds almost all the time in these patients, because even though I see something in the uterus, that doesn’t necessarily always rule out the fact that there could also be an ectopic pregnancy. 07:48 So go ahead, think about this. 07:50 You may or may not ever see it. 07:52 It’s a relatively rare diagnosis. 07:54 But it’s something that can be very life threatening to the patient.
About the Lecture
The lecture Ectopic Pregnancy: Diagnosis by Sharon Bord, MD is from the course Abdominal and Genitourinary Emergencies.
Included Quiz Questions
In a normal intrauterine pregnancy (IUP) a transvaginal ultrasound will first be able to document this at what level of HCG?
- 1000–2000 mIU/ml
- 800–1000 mIU/ml
- 600–800 mIU/ml
- 400–600 mIU/ml
- 200–400 mIU/ml
What medication must be given to women with a negative Rh-blood type to prevent future Rh incompatibilities?
- RhoGam [anti-D (Rh0) immunoglobulin]
- Tdap
- Anti-HbS
- Anti-tetanus
- O negative blood
What is the first-line imaging modality for patients with ectopic pregnancy?
- Ultrasound
- Plain film x-ray
- CT scan
- MRI
- Angiogram
What is a heterotopic pregnancy?
- The simultaneous occurrence of an intrauterine pregnancy and an ectopic pregnancy
- Two or more intrauterine pregnancies
- Implantation of the embryo in the fallopian tube
- Two or more ectopic pregnancies
- Implantation of the embryo in the abdominal cavity
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |