Playlist
Show Playlist
Hide Playlist
Ectopic Pregnancy: Definition and Treatment
-
Slides Ectopic Pregnancy.pdf
-
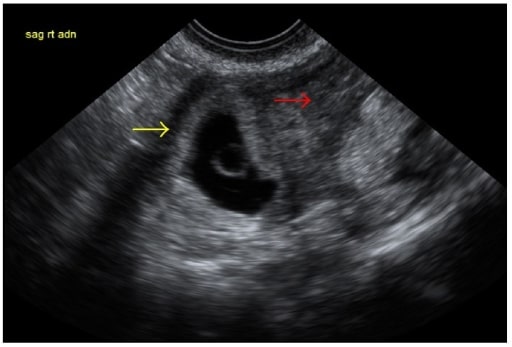
Download Lecture Overview
00:01 In this lecture, I'll be reviewing ectopic pregnancy. 00:04 This is important for you to listen to as you can see questions on your USLME. 00:10 In addition, you can save a life by understanding the pathophysiology of an ectopic pregnancy. 00:18 An ectopic pregnancy essentially is a pregnancy that is developing outside of the uterus. 00:24 This can happen in several locations. 00:27 Let's review some of those locations now. 00:29 An ectopic pregnancy is more likely to occur in the ampulla. 00:34 Over 70% of ectopic pregnancies occur here. 00:38 Do you know why? I'll wait for you to answer that. 00:49 If you guessed because fertilization occurs here then you are correct. 00:55 There are other regions that an ectopic pregnancy can implant including the isthmus and the fimbria. 01:03 3% of all ectopics occur on the ovary. Sometimes you can have an ectopic in the interstitium. 01:11 This is the junction between the tube and the uterus. 1% of all ectopics are abdominal. 01:18 This is extremely rare. However, we are seeing a surge in cervical ectopics. 01:25 These ectopics can be life-threatening as sometimes they look like a miscarriage. 01:30 And if you try to extract them, the patient can lose her blood supply very quickly. 01:36 And this is very life threatening. 01:39 An ectopic pregnancy looks like this upon laparoscopy. 01:42 They account for 1% to 2% of all pregnancies. 01:45 They account for 5% of all assisted reproductive technology pregnancies. 01:50 For more information about ART, please refer to that lecture slide. 01:56 There are some definitive risk factors for an ectopic pregnancy such as previous surgery on the tube. 02:03 Any surgery but especially tubal ligation can cause ectopics to occur. 02:09 Tubal pathology from pelvic infection such as PID can also lead to ectopic. 02:15 DES exposure increases the risk five-fold. 02:19 However, less patients exposed to DES are now in their perimenopause and menopausal stages. 02:25 So, you're unlikely to see this but you may be tested on your exam. 02:30 Also, patients who have infertility who have any type of ART are two-fold increased risks. 02:37 They are more likely to have a heterotopic. 02:39 That means one ectopic and one normal intrauterine pregnancy or IUP. 02:45 Patients who smoke are more likely to have an ectopic. 02:50 There's a two-fold increased risk. 02:52 So, you should encourage all of your patients to stop smoking for their own health benefit but of course, for the benefit of any pregnancy that may occur. 03:01 Contraception, we think that taking contraception decreases the incidence or absolute risk of ectopic. 03:07 However, there are some times when the contraceptive method may fail and there's an increased risk of ectopic if you conceived with an IUD in place. 03:18 Again, if you've had permanent sterilization, these patients are more likely to have ectopic if they become pregnant after the sterilization. 03:26 One third of pregnancies from sterilization are an ectopic. The diagnosis is easy. 03:33 A beta positive hCG usually occurs eight to ten days after ovulation. 03:38 There is some time that is required to determine what the character of the beta-hCG will be. 03:44 Will it double normally every two to three days or will it plateau? Serial beta-hCG determinations are more difficult to interpret in the setting of ART possibly because there may be more than one gestation and therefore, the beta-hCG is elevated. 04:03 Let's now look at what a normal pregnancy looks like. 04:06 With an IUP, you have a gestational sac usually at 38 days after the onset of menses. 04:15 Then, you should see a fetal pole and a yolk sac. 04:19 Perhaps, you'll see the yolk sac such as the one pictured here, which is an indication that there is an intrauterine pregnancy. 04:27 However, you can't see a yolk sac in the adnexa. 04:30 So, it's important to look at the ultrasound pictures to determine where the yolk sac and therefore the IUP should be. An abnormal pregnancy would actually look like this. 04:41 This is an observation of a gestational sac with a yolk sac, an embryo, and fetal cardiac activity outside of the uterus. 04:48 This establishes the diagnosis of an ectopic. 04:51 Typically, we don't always see very well like the last image. 04:58 So, sometimes if we suspect an abnormal pregnancy which could be an abnormal IUP, intrauterine pregnancy or an ectopic, we recommend doing some type of uterine curettage. 05:09 This can be done with manual vacuum aspiration or a dilation and curettage. 05:14 We typically do this when the beta-hCG is above the discriminatory zone but there is no IUP seen on ultrasound. 05:22 Typically, if you recover villi, this will exclude ectopic and will tell you it was an abnormal IUP. 05:28 However, it does not rule out the chance of a heterotopic. 05:32 Let's talk about the medical management of ectopic pregnancy. 05:36 Methotrexate is an effective first-line medical therapy. 05:39 It works by inactivating dihydrofolate reductase and inhibiting DNA and RNA synthesis. 05:46 It is the preferred alternative to surgical treatment. 05:49 The dosage depends on the protocol. 05:51 A single dose and two doses correspond to 50 mg/m2 of body surface area. 05:57 For the protocol with two doses, one dose is given on day 1, and the other on day 4. 06:03 For the multiple dose protocol, 1mg/kg/day is given on days 1, 3, 5 and 7. 06:11 However, the patient needs to meet some criteria. She needs to be hemodynamically stable. 06:17 She must not have any evidence of acute or intra-abdominal bleeding. 06:21 And she must be compliant with the medication and is scheduled to come back to check her titers of beta-hCG. 06:29 Methotrexate does have some contraindications. 06:33 If the woman is currently breastfeeding, she cannot take Methotrexate. 06:37 If she's immunodeficient such as HIV positive or has AIDS, she is not a candidate for Methotrexate. 06:45 If the patient has cirrhosis or hepatitis, she is not a candidate for Methotrexate. 06:50 If she has renal failure, she should not receive Methotrexate. 06:54 Any bleeding dyscrasias or blood dyscrasias are also a contraindication. 06:59 And sometimes patients report a history of sensitivity to Methotrexate. 07:03 They should also not receive Methotrexate. 07:07 Any active pulmonary disease such as an ongoing asthma exacerbation should not permit the use of Methotrexate in these patients. 07:16 Also, if a patient has active peptic ulcer disease, she should not receive Methotrexate to treat her ectopic. 07:23 I'd now like to review the surgical treatment for ectopic pregnancy. 07:27 We traditionally do this via laparoscopy and not laparotomy. 07:32 I can either perform a salpingostomy or a salpingectomy. 07:37 A salpingostomy allows me to make a linear antimesenteric incision on the fallopian tube. 07:44 Then I remove the ectopic pregnancy through the incision sometimes with hydrodissection. 07:50 The incision is then allowed to close by secondary intention. 07:54 For a salpingectomy, the entire tube is removed. 07:58 With salpingectomy, we try to avoid this so the patient can have access to both her tubes even after having an ectopic. 08:06 About 65% of patients who've had an ectopic in a tube will go on to have an IUP or an intrauterine pregnancy. 08:14 Thank you for listening and good luck on your exam.
About the Lecture
The lecture Ectopic Pregnancy: Definition and Treatment by Lynae Brayboy, MD is from the course Female Pelvic Medicine. It contains the following chapters:
- Ectopic Pregnancy: Definition and Risk Factors
- Methotrexate (MTX): Indications and Contraindications
Included Quiz Questions
What is the most common location of implantation of an ectopic pregnancy?
- Ampulla
- Isthmus
- Fimbriae
- Ovary
- Interstitium
Which of the following establishes the diagnosis of an ectopic pregnancy?
- Observation by ultrasound of a gestational sac with a yolk sac, embryo, or fetal cardiac activity outside of the uterus.
- A positive pregnancy test after ART.
- Serial testing showing increasing beta-hCG levels.
- Ultrasound confirmed absence of a gestational sac in the uterus with an equivocal pregnancy test result.
- The lack of fetal cardiac activity at six weeks of gestation.
What is the first-line medical treatment for ectopic pregnancy?
- Methotrexate
- Mifepristone
- Misoprostol
- Dinoprostone
- Oxytocin
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |