Playlist
Show Playlist
Hide Playlist
Diverticulitis: Management
-
Slides Diverticulitis General Surgery.pdf
-
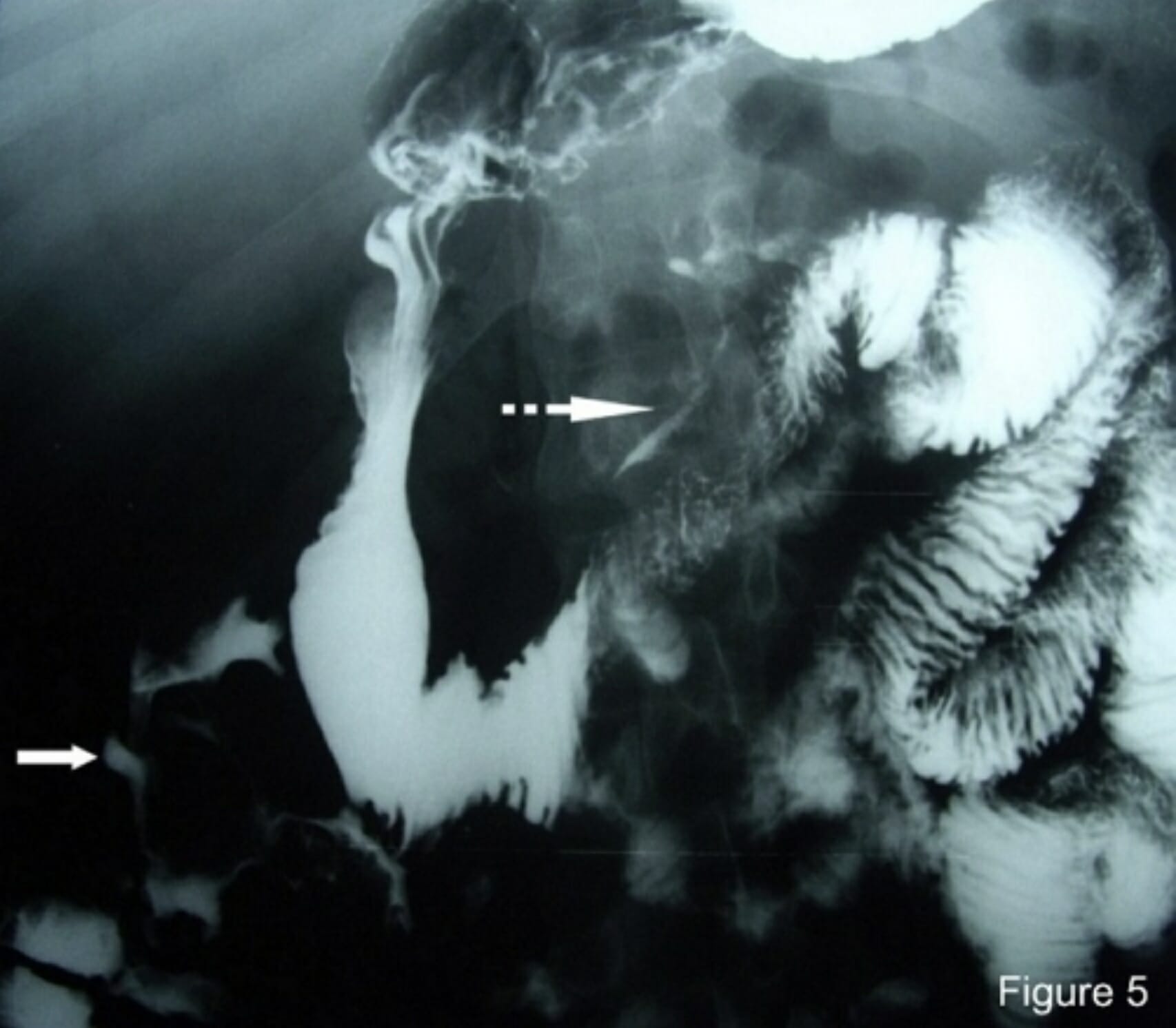
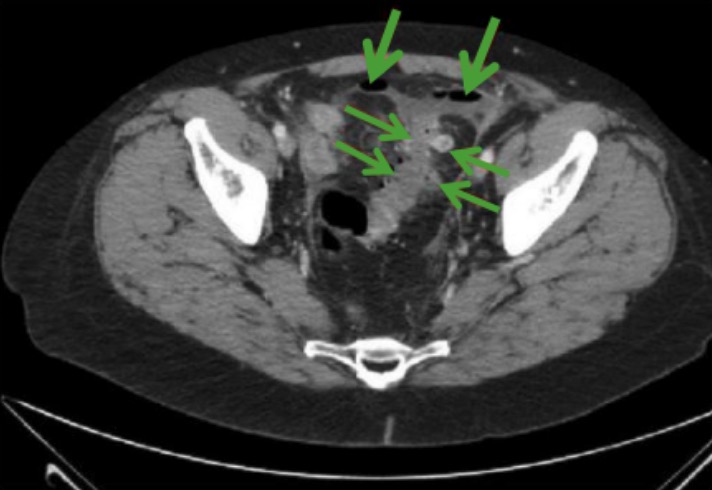
Download Lecture Overview
00:01 Let’s discuss the management of diverticulitis based on the Hinchey classification. Remember, Hinchey 1 through 4 is a continuous spectrum of severity of disease. Hinchey 1 is the simplest to take care of. 00:15 We usually can advance diet fairly quickly as soon as the patient’s symptoms resolve. That means the resolution of pain. We keep the patient on the antibiotics to cover the colonic flora. 00:28 We wait for symptomatic relief. When the patient feels better, we advance the diet. We discharge the patient. 00:36 Remember, for Hinchey 1 classification patients, oftentimes many of these people can be observed and managed in an outpatient setting. How about Hinchey 2-4? Well, these are a little bit more complex than the Hinchey 1 patients. They may require interventional percutaneous drainage of the abscess. 00:56 Recall that Hinchey 2 have a pericolonic abscess formation. These abscesses unfortunately have very poor antibiotic penetration. For us to get surgical source control, usually we have to call a radiologist. 01:09 Now, on the examination presented with the scenario of a patient who comes in with a Hinchey 2-4 classification, as long as the patient does not have any rebounds or guardings suggestive of peritoneal signs, the patient can be safely managed with antibiotics and interventional percutaneous drainage. However, if the patient’s disease progresses, interventional radiologists are not available, or the interventional percutaneous drainage is not successful in the drainage, the patient may require surgery particularly with clinical deterioration. If you decide surgery is necessary and it’s important to stress that surgery is not first line therapy for diverticulitis, antibiotics are. We usually reserve surgery for patients who have severe complications of diverticulitis or failure of progression or resolution based on nonoperative management. But should surgery become a necessity then we want to discuss what the surgical options are. In this slide, you’ll notice that a black box around the sigmoid colon has been outlined. Let’s say that this black box is the area that’s affected by diverticulitis. 02:21 Resection limits usually require us to go down past the sigmoid-rectal junction, not necessarily peritoneal reflection. Proximally, we want to get to a point of soft, viable healthy colon. Remember, it’s not necessary to get rid of all diverticular disease as diverticulosis may be quite scattered throughout the entire length of the colon. Generally speaking, it’s safe to perform a primary anastomosis after the resection as long as it’s not an emergency situation. During emergency, it may be necessary to do a temporary ostomy. How do we guard against diverticulitis? We don’t really know. 03:05 Based on some evidence, that low fiber diet and left side of predominance suggest that there is a high intraluminal pressure related to diverticulosis and subsequent diverticulitis. 03:16 Generally, we recommend a high-fiber diet and keeping our bowel movements regular and soflty-formed. 03:24 But it’s questionable if seeds and nuts exacerbate the disease. Traditional teaching has always been avoid corn, popcorn, things that may “get stuck in one of the diverticulum." But no scientific evidence has ever proven that to be the case. Some important clinical pearls: Patients should undergo colonoscopy to exclude cancer. Remember, prior to surgery, it’s absolutely particularly in patients who are within an age group to exclude cancer prior to doing definitive therapy for diverticulosis or diverticulitis. The number of episodes of diverticulitis is no longer an important determinant of the necessity for surgery. It used to be that in young patients, we would offer surgery after the second episode. One of the fears is that the subsequent episodes of diverticulitis may be clinically more severe and may require emergency surgery. Further studies have demonstrated that not to be the case. The decision to pursue surgery for diverticulitis is a very personal one between the patient and the surgeon. Here are some complications that most likely would require surgery and this is high-yield information for the examination: bleeding, obstruction, perforation, and septic shock. Recall that bleeding is much more common in diverticulosis than diverticulitis but one can bleed and one can bleed significantly from diverticular disease. If the patient has localizable bleeding then regional resection is reasonable. Bleeding patients who undergo massive transfusions in excess of six units of packed red blood cells or who become hemodynamically unstable will likely require a surgery. Patients who have a bowel obstruction, large bowel obstruction as a result of diverticulitis likely have developed a phlegmon significant enough to cause proximal dilation. 05:24 Some indications of operation for large colon obstruction are patients who have signs of small bowel obstruction, cecal dilation. As you know, the cecum is the thinnest portion of the colon and governed by LaPlace’s law, also the most likely area to perforate. Frank perforations in excess of the microperforations in significant pneumoperitoneum is an indication for surgery. Finally, septic shock in a patient who’s clinically deteriorating. One of the other complications that can result from diverticulitis is an anomalous connection between the colon and the bladder. This is called the colovesical fistula. You notice on these images that there is air in the bladder filled with contrast fluid where there should be rarely any air in the bladder. This is called pneumaturia. A colovesical fistula can result or present itself firstly with pneumaturia. Patients will often present complaining of interruptions of the voiding stream with pockets of air. Additionally, frequent urinary tract infection may lead you to believe that the patient has a colovesical fistula. How do we manage colovesical fistulas? Recall, a fistula is an abnormal connection between two epithelialized surfaces. 06:48 In this situation, it’s between the colon and the bladder. There’s only one way to fix that problem and that’s surgically. What we want to do intraoperatively is to break down the fistula. 07:00 The connection between the colon and the bladder needs to be separated. Once separated, the hole in the bladder is repaired. Some high-yield information for your USMLE examination: Remember, many uncomplicated diverticulitis cases can be treated with oral antibiotics as outpatient alone. 07:20 Many of these patients don’t need to be admitted into the hospital. Recall that the number of episodes of diverticulitis is no longer in and of itself an indication for surgery. Lastly, if your patient is decompensating as is the case in any question or scenario, the answer choice usually involves operating on that patient. Thank you very much joining me on this discussion of acute diverticulitis.
About the Lecture
The lecture Diverticulitis: Management by Kevin Pei, MD is from the course General Surgery.
Included Quiz Questions
Which of the following is NOT typically part of the management of Hinchey Class 1 diverticulitis?
- Percutaneous phlegmon drainage
- Early alimentation
- Antibiotics
- Dietary modification recommendations
- Outpatient management and follow up
Which of the following is NOT an indication for surgical intervention in patients with diverticulitis?
- Presence of pericolic phlegmon
- Intestinal bleeding
- Presence of a walled-off abscess without access to interventional radiology
- Failure of percutaneous drainage
- Septic shock
Complications of diverticulitis include all of the following EXCEPT?
- Cancer
- Intestinal bleeding
- Obstruction
- Colovesicular fistula
- Bowel perforation
Customer reviews
4,5 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
1 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Very useful, practical I've met a pt of diverticulitis but was mis-diagnosed as appendicitis
I would have liked to also learn a bit about Hartmans procedure in emergent cases. Discussion of recurrence rates for patients undergoing conservative management