Playlist
Show Playlist
Hide Playlist
Diabetes Insipidus (DI) in Children
-
Slides DIandSIADH Pediatrics.pdf
-
Download Lecture Overview
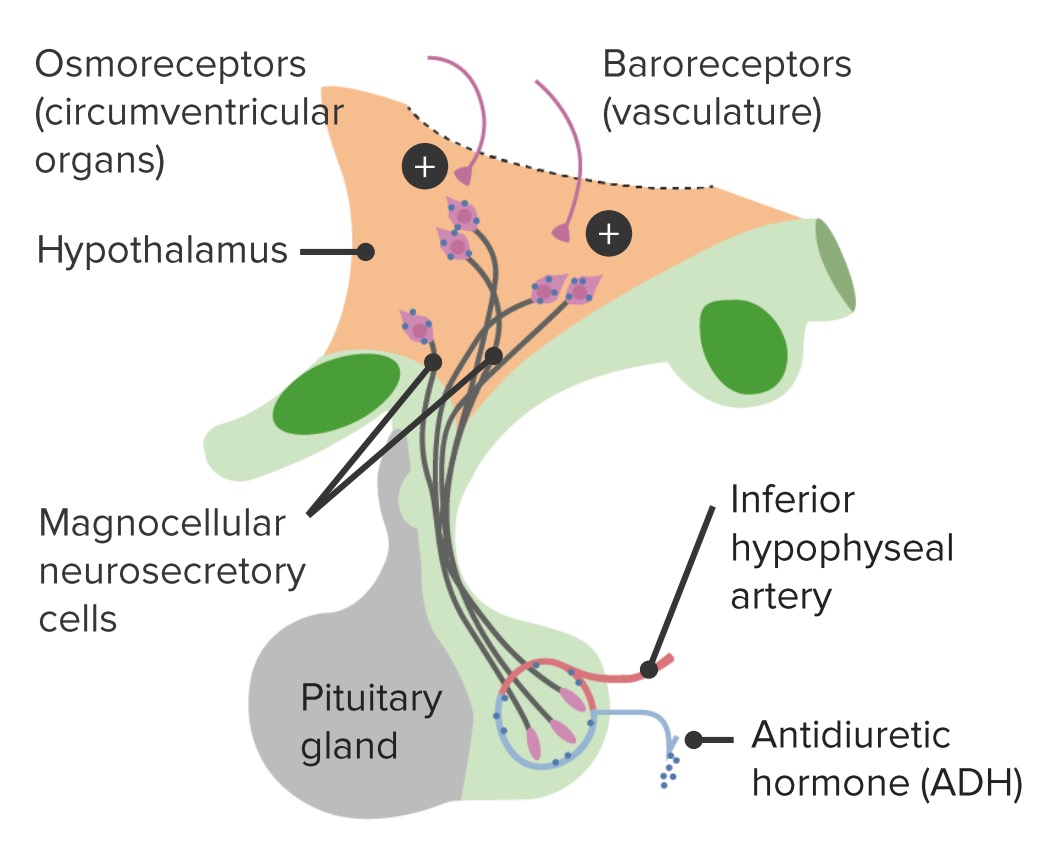
00:01 In this talk we're going to discuss diabetes insipidus SIADH will be covered in a separate lecture. 00:07 This is a problem with too little and too much antidiuretic hormone. 00:13 So let?s remember about antidiuretic hormone sometimes called vasopressin. 00:18 This is secreted by the posterior pituitary, it causes an insertion of aquaporin into the distal collecting duct of the kidney. 00:27 Remember that collecting duct, the tissue around it is very concentrated, so when those aquaporin are placed in the water will resorbed out of the urine. 00:38 Antidiuretics hormone concentrates the urine. 00:43 So diabetes insipidus is a problem whether is decreased ADH secretion from the posterior pituitary. 00:52 That is called Arginine vasopressin deficiency (AVP-D), previously called central DI or central diabetes insipidus. 01:01 This can be cause from a damaged hypothalamus or a posterior pituitary. 01:07 There's a lots of conditions that can do this, unusual ones like granulomatosis with polyangiitis (previously called Wegener's granulomatosis) which you would see in the patient who has a coughing up blood and it's urinating blood. 01:20 Sometimes it happens in the newborn who have problems around the birthing period or gonna happen in patients with sickle cell disease or with other risk of clots forming inside the brain or could happen with trauma. 01:32 Alternatively, patients could have Arginine vasopressin V2 resistance (AVP-R), previously called nephrogenic diabetes insipidus. 01:41 In this case they have the ADH being secreted by the posterior pituitary but the problem is the kidney isn't responding to it. 01:50 So either one of these problems is gonna result in excessive urination and that excessive urination leads a patient to develop a high sodium, and it's the high sodium that gets patients in trouble. 02:06 So let?s look drill down on causes of central diabetes insipidus. 02:12 We see it commonly in children with significant developmental abnormalities of the brain. 02:19 We'll see it in patients with injury to their hypothalamus, or their pituitary gland, patients with pituitary tumors. 02:25 A patient with meningitis or encephalitis may develop damage to their pituitary gland. 02:32 Rarely things like Wegener?s or histiocytosis, there can be some rare genetic syndromes where patients develop diabetes insipidus. 02:42 This is familial diabetes insipidus and of course after brain surgery. 02:47 This is to be compared differently to patients who have nephrogenic DI. 02:53 There are genetic receptor or aquaporin mutations that exist in the community. 02:59 Patients with chronic renal disease may develop in nephrogenic DI and certainly renal malformations of the patient has a bad bilateral vesicoureteral reflux for example they may develop nephrogenic DI. 03:13 Also remember medications and if it's on your test it's gonna be lithium. 03:18 Lithium which is treated usually, use to treat bipolar disease and other psychiatric conditions has the consequence of nephrogenic diabetes insipidus. 03:28 There's others that do as well though like amphoteracin which has such bad side effects, sometimes we just call it amphoterrible. 03:36 Clozapine which is an antipsychotic and foscarnet which is an antiviral sometimes used for resistant cytomegalovirus, though newer antivirals are now more commonly preferred. 03:48 I've never use foscarnet in my career, it's very rare to use that in children but all of these are the medicines that are accused of causing nephrogenic diabetes insipidus. 03:58 Unlike foscarnet, the more commonly used antivirals for CMV such as ganciclovir and valganciclovir do not typically cause nephrogenic diabetes insipidus, though they may have other renal effects. 04:13 So regardless of whether it's central or nephrogenic, how does diabetes insipidus present? Well, quite simply they pee a lot. 04:22 These patients are gonna have significant polyuria and if they're cognitively intact will accommodate that by having polydipsia. 04:31 They're going to be drinking a lot. 04:33 In patients with significant brain disease who can't mount thirst or lack the ability to drink for themselves. 04:40 It's common for them to present with severe dehydration because they aren't able to regulate their own water level inside their blood. 04:51 These patients have a challenge, very challenging to take care of. 04:56 So look for signs of systemic diseases as well that might be resulting in DI. 05:03 For example, Wegener?s. 05:06 Central DI after surgery or trauma is interesting and it may come upon a test that there's a classical triple phase response to trauma and surgery. 05:18 We think they're going to have a problem suddenly we feel like it's all turned out okay and then we discover they do in fact have a problem. 05:27 So after the surgery from maybe one to four days, patients will have, in a sense a stunned, the posterior pituitary. 05:35 It does not want to release antidiuretic hormone, so these patients will have a polyuric phase they will be peeing frequently. 05:45 Then that stored ADH that was there prior to the damaged to the pituitary or the hypothalamus, suddenly is released and these patients will have a period when they are less polyuric or they're peeing normally. 06:02 After that as they are now no longer able to permanently make ADH they go back into their polyuric phase then we call this the permanent polyuric phase. 06:12 So just remember these three phases in particular for patients who had trauma to the pituitary gland or if had surgery. 06:21 So causes of diabetes insipidus and the symptoms they might be having, CNS tumors patients may present with morning headaches, visual changes, or poor school performance. 06:33 For Wegener?s disease they'll present with hemoptysis and hematuria. 06:37 For vascular injuries especially in sickle cell patients will know they have sickle cell, they'll have all the findings of pain crisis and all the other problems that occur. 06:47 Also patients who are hypercoagulable who have a vascular injury, may have clots and other problems as a result of their hypercoagulability. 06:57 In neonates often times there's a story of a bad peripartum experience. 07:02 Let's fix [inaudible], whether incapable of breathing well and that cause the central neuronal injury of the pituitary gland. 07:10 Patients with congenital hypopituitarism typically present with other problems as well related to their pituitary gland. 07:17 They may develop hypoglycemia as a result of problems with their HPA axis, or micropenis due to issues with their HPG axis. 07:27 And then with patients with familial diabetes insipidus we would expect to hear a family history that the parent or someone related to them also has that condition. 07:37 So in patients with an intact thirst mechanism, the diagnosis of the disease is largely through a history because these patients are drinking adequately to maintain a normal serum sodium and normal labs. 07:58 However, if we are going to test for diabetes insipidus we will typically measure serum and urine osmolality. 08:07 In a patient with uncheck diabetes insipidus we expect high serum osms of more than 300 and low urine osms with the dilute urine. 08:18 If we are unclear if they have diabetes insipidus or some other problems say, psychogenic polydipsia we may do a water deprivation test. 08:28 In patients with DI, a water deprivation test is dangerous these patients can dehydrate very quickly. 08:38 So we need to watch them very carefully in a controlled in-patients setting when we stop them from drinking and measure serially their blood levels of sodium to make sure they're not getting in too much trouble. 08:50 In patients where we suspect something might be wrong with pituitary an MRI of the brain with pituitary cut downs like you can see in this patient here with an abnormality of their pituitary gland is indicated. 09:02 If a patient has DI we're simply treating it with oral hydration. 09:09 Children who can't regulate their own drinking are in grave danger and we worry about it. 09:16 If a patient has central DI they'll be responding to administer DDAVP. 09:23 So we can give DDAVP in two different ways, we can administer it nasally as a spray or we can give it orally. 09:32 The nasal medication is rapid onset chronically it can cause some damage to the oral mucosa and as a result, it's not a particularly good way to start off the drug for infants. 09:44 Orally, it's a little bit slower onset, there's variable GI absorption so we have to track these children and see how they're responding to the drug. 09:52 It's a lot easier for parents to administer to infants. 09:56 SubQ or IV DDAVP is available but only really use if a patient is unable for some reason to take it either orally or nasally.
About the Lecture
The lecture Diabetes Insipidus (DI) in Children by Brian Alverson, MD is from the course Pediatric Endocrinology. It contains the following chapters:
- Pathology
- Signs & Symptoms
- Diagnosis & Management
Included Quiz Questions
Which of the following has the strongest association with diabetes insipidus?
- Granulomatosis with polyangiitis
- William’s syndrome
- Down’s syndrome
- Adult onset IDDM
- Jarcho-Levin syndrome
Which of the following is NOT a common cause of drug-Induced nephrogenic Diabetes insipidus?
- Didanosine
- Amphotericin B
- Lithium
- Foscarnet
- Clozapine
Which of the following best describes the triple-phase response by the posterior pituitary after trauma or surgery to the brain?
- Polyuric phase - Normal urination - Polyuric phase (chronic)
- Anuric phase - Normal urination
- Normal urination - Anuric phase - Polyuric phase
- Normal urination - Polyuric phase - Anuric phase
- Anuric phase - Normal urination - Anuric phase
A 12-year-old boy presents with polyuria for the last 3 months. His other complaints include morning headaches and recent problems with vision. Which of the following is the most likely cause of his symptoms?
- CNS tumor
- Wegener's Granulomatosis
- Familial Diabetes Incipidus
- Congenital hypopituitarism
- Sickle cell disease
Which of the following values are consistent with Diabetes Insipidus?
- Serum Osm > 300 mOsm/kg and Urine Osm < 300 mOsm/kg
- Serum Osm < 300 mOsm/kg and Urine Osm < 300 mOsm/kg
- Serum Osm > 300 mOsm/kg and Urine Osm > 300 mOsm/kg
- Serum Osm < 300 mOsm/kg and Urine Osm > 300 mOsm/kg
- Serum Osm < 250 mOsm/kg and Urine Osm < 150 mOsm/kg
A 14-year-old girl is brought to the pediatrician due to excessive urination. As your suspicion of Diabetes insipidus is confirmed by lab test, which of the following additional tests might be helpful in distinguishing between central from nephrogenic DI?
- Water deprivation test followed by ADH administration
- Random Serum and Urine osmolarity
- Water deprivation test followed by Cortisol administration
- Oral glucose loading with measurement of Urinary glucose
- Brain MRI
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Excellent lecture, once more a complex topic made easy. Thanks! It ties well physiology with pathophysiology with diagnosis and treatment. Seamless.