Playlist
Show Playlist
Hide Playlist
Definition and Etiology – Pericarditis
-
Slides Myocarditis Pericarditis.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
00:00 Welcome back. We’re going to talk about structures that are just very slightly outside of the heart, that is to say the pericardium, and diseases mostly inflammatory and some infectious diseases and how they impact myocardial cardiac function. The normal pericardium is a very thin layer of mesothelial cells that sit on a basement membrane. 00:25 As a higher power blowup, what we’re looking at here we have the endocardium that faces to the inside of the ventricle, that’s where the blood is going to be, that’s going to be endothelial cells. And then we have the myocardium, a combination of cardiac myocytes, fibroblasts, endothelial cells being formed in capillaries, etc. and then a few inflammatory cells. And then we get into the visceral pericardium. So, there are actually 2 layers of the pericardium. We have a pericardial layer where the mesothelial cells are sitting on the basement membrane and fibrous connective tissue that’s tightly applied to the heart, that’s the visceral pericardium. And then it folds over and around, that’s going to form the parietal pericardium. There is a virtual space between the visceral and the parietal pericardium that normally contains 5 to 10 cc of serous fluid. 01:17 That’s normal. And the thought is that little bit of fluid allows some lubrication of the heart in the pericardial sac. Inflammation of the pericardium, basically is pericarditis, that’s the definition. And we’re going to inflame that lining, and it can be involved just the visceral pericardium, the parietal pericardium or, in most cases, both layers. We will see dilated and leaky vessels. So we will see accumulated fluid because that’s the nature of acute inflammation. And we will see inflammatory cells. And, depending on the tempo and how long the pericarditis has been around, we may see predominantly neutrophils or we may see predominantly mononuclear inflammatory cells like lymphocytes and macrophages where we may see some combination thereof. The etiologies of pericarditis, in many cases, we don’t know. It’s idiopathic. But we do have some other causes that we are well aware of that are causally associated in many cases. So, viral pericarditis is is actually reasonably common particularly in certain seasons where their viruses are spreading around, Coxsackie B virus, influenza virus, HIV in the appropriate individual and echovirus are all causes of a viral pericarditis and can be probably the more common causes of pericarditis. We can also have bacterial causes. If we’re going to look at bacterial causes of pericarditis, the most common worldwide is going to be tuberculosis. 02:52 In developed countries, industrialized countries, that’s a relatively rare cause. And other bacterial causes include pseudomonas in the appropriate immunocompromised host, staphylococcus species, streptococcus species, mycoplasma kind of atypical pericarditis, Lyme disease. Lyme pericarditis can occur with spirochetes. And we can also have fungal pericarditis, Histoplasma, blastomycosis, Coccidioides immitis and aspergillus. So, depending on the host, the geographic location and various other things, we may have different organisms that we may invoke. There can also be autoimmune causes of pericarditis. So, we can have inflammation that’s specifically or preferentially involves the pericardium because of the antigenic differences that are there. And these include autoimmune diseases such as lupus erythematosus, rheumatoid arthritis, sarcoidosis, and various vasculitides such as Behcet’s disase and Takayasu’s arteritis. Metabolic causes of pericarditis include uremia. And when patients have renal failure, there can be an increased vascular permeability particularly in the pericardium with some associated inflammation and we attribute that to various non-metabolism of certain things that would normally be cleared by the kidney. 04:20 Hypothyroidism is also an interesting form of metabolic pericarditis. The etiology is not well understood but can be a cause. Perhaps the more common causes of pericarditis are non-infectious and include things like chronic congestive heart failure where you can have chronic transudation of fluids because of venous congestion and poor cardiac function. Dressler’s syndrome is an interesting one that’s associated with either prior surgery on the heart or prior myocardial infarction. The surgery on the heart or the myocardial infarction elicits certain neoantigens that aren’t normally seen or responds to those neoantigens can give rise to a pericarditis, tends to be transient, tends to be very responsive to immunosuppression, steroids or even aspirin anti-inflammatories. 05:14 That’s Dressler’s syndrome. You can have pericarditis associated with the aortic dissection. So if you have retrograde dissection that involves the pericardial sac, irritation inflammation there, provided it’s not an overwhelming dissection with an overwhelming volume that causes death, can give rise to a pericarditis.Takotsubo cardiomyopathy, so-called broken heart syndrome, stress cardiomyopathy due to elevated levels of catechols causing focal injury to the heart, and it’s that inflammation associated with the focal microscopic infarction of Takotsubo that will give rise to the pericarditis. Cancer is an important one. So, cancer is not confined to any particular tissue, and if it’s metastatic disease, either solid malignancy or hematologic malignancy, it can end up in the pericardium, the inflammation associated with that cancer or vasoactive mediators elaborated by that cancer can drive effusions and can induce inflammation that will manifest this pericarditis. So, malignant pericarditis is an important etiology. There are some drugs that can also manifest with a pericarditis. It’s idiosyncratic. 06:30 The actual mechanism is not understood although some of the drugs may act as a hapten to induce an immune-mediated pericarditis, kind of like a lupus, for example. 06:41 So, procainamide, hydralazine, isoniazid use to treat tuberculosis, various chemotherapies and certainly radiation can all induce injury inflammation involving the pericardium.
About the Lecture
The lecture Definition and Etiology – Pericarditis by Richard Mitchell, MD, PhD is from the course Myocarditis and Pericarditis.
Included Quiz Questions
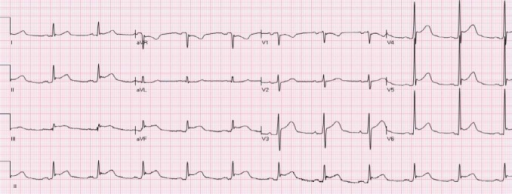
What defines pericarditis?
- Inflammation of the lining surrounding the heart
- Inflammation of the muscular layer of the heart
- Absent p wave
- Absent QRS
- Prolonged PR segment
What is the most common bacterial cause of pericarditis?
- Tuberculosis
- Pseudomonas
- Staphylococcus
- Influenza
- Coxsackie
What medication is most strongly associated with pericarditis?
- Hydralazine
- Amoxicillin
- Penicillin
- Cyclophosphamide
- Carboplatin
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |