Playlist
Show Playlist
Hide Playlist
Crystalline Arthropathies: Gout / Pseudogout
-
Rheumatology I 01 Non-Autoimmune Arthritis.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
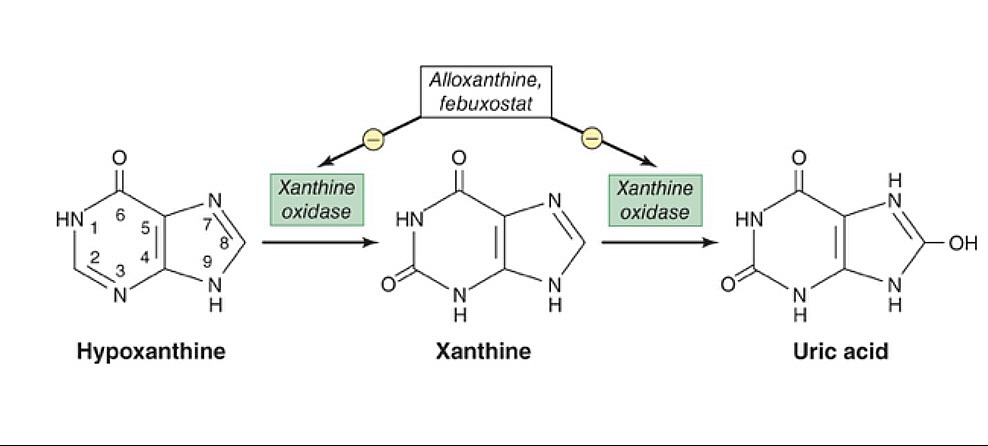
00:02 Continuing our discussion in rheumatology. 00:03 This time we'll take a look at crystalline arthropathies. 00:07 Now, you've commonly probably come to encounter gout versus pseudogout. 00:12 But we need to be more technical. 00:15 So, pseudogout, referred to, as we shall see, calcium pyrophosphate deposition disease, and prior to going into or diving into detail, we'll take a look at gout, first. 00:28 So, what is gout, by definition? By definition, gout is uric acid accumulating in your body. 00:36 How did it accumulate? 90% of your patients with gout have a hard time excreting the uric acid from the kidney. 00:45 90% of the time. 00:47 Now, with that 90%, most of your patients will be idiopathic. 00:53 Now, could renal failure result in lack of excretion? Sure. It could contribute. 01:00 Next, we'll take gout and then we'll divide it into acute and chronic, that's important. 01:05 And by acute and chronic, remember, we begun begin the discussion on rheumatology by discussing the timeline. 01:10 And then we said that 6 weeks was the magic number. 01:13 You start getting into greater than 6 weeks, then you're getting into chronic category, aren't you? So, gout is acute. 01:20 It's inflammatory, no doubt, all right? So, this is inflammatory. 01:24 Then you're going to accumulate these monosodium urate crystals. 01:28 That's the operative word. You see that? MSU, monosodium urate crystals. That's what you're focusing on. 01:35 Where is it accumulating? In different parts of the body. 01:39 For example, commonly here, the patient, who's usually a male, is going to be complaining of pain, where? Let's say watching a football game and then having a beer, and all of a sudden, complains of pain in the big toe, called podagra. 01:56 Acute, inflammatory, monoarticular. 01:59 What's that mean? One joint, asymmetric. 02:02 Not both big toes, one big toe. 02:05 "Oh, my goodness, Doc. 02:07 It's my right toe that's in excruciating pain." I'll give you alcohol there on purpose. 02:13 I'll tell you why as we move forward. Welcome to gout. 02:18 What exactly are we accumulating? What we're accumulating in this picture showing is monosodium urate crystals. 02:25 This may then accumulate in the big toe, called the metatarsophalangeal joint. 02:30 Or maybe perhaps it accumulates in your tissue. 02:34 When it accumulates in your tissue, let me tell you, it's then called tophaceous gout. 02:37 Or you've heard of tophi. 02:39 But the point is, it's accumulating uric acid. 02:44 That's the genesis. So what then happens? What's causing that pain? Well, let's say that the patient idiopathically is unable to properly get rid of uric acid, right? So now these monosodium urate crystals are accumulating in your joint. 02:58 Now it's an antigen. 03:00 So then what are you going to do? Well, just like any antigen, you're going to immediately, then, respond with an inflammatory response. 03:07 The phagycitic cells, the neutrophils and such, are going to try to come in and at these wonderful crystals. 03:13 Not too successful, because now these neutrophils are then going to release cytokines and such. 03:20 And these cytokines are then going to cause quite a bit of pain, as you can imagine. 03:24 So, therefore, what you're focusing upon is the fact that the activation of inflammasome. 03:31 Whereas inflammasome will not necessarily be asked about, but understand it will contribute to the pain. So ultimately, what does that mean to you? In acute gout, what are you trying to do? You're trying to lessen the pain in this patient, aren't you? You lessen the pain by giving anti- inflammatory drugs, don't you? For example, NSAIDs or maybe colchicine. 03:54 What do they have in common? Both are acute anti-inflammatory agents. 04:00 Something that you want to keep in mind because you're trying to prevent the cytokines from causing pain in your patient. 04:08 Pathogenesis, we said that your patients are accumulating uric acid. Hyperuricemia. 04:15 The definition, uric acid of > 6.8 mg/dL. 04:19 Highlight that. Keep that in mind. 04:22 Disorders of uric acid, as I told you, could be the overproducers, but 90% will be the under-excreters. 04:30 You understand the definition? The kidneys are unable to properly get rid of the uric acid. 04:37 What about the overproduction? Easily 10%. 04:40 Important? Oh, yeah. 04:41 What if you have a patient that has cancer receiving chemotherapy? What do you know about cancer? Neoplasia, increased proliferation of these cells. 04:50 And these cells are still made up of DNA, are they not? Because what is uric acid, biochemically, please? It is a breakdown product of purine. 04:59 And so, therefore, if the patient receiving chemotherapy, you are then causing lysis of the tumor, therefore releasing quite a bit of uric acid called tumor lysis syndrome. 05:10 That would come under which category? Under-excretion, overproduction? Technically, overproduction. Talk a little bit more. 05:17 As I told you, under-excreters will be 90% of your patients. 05:20 Why? Idiopathic predominantly, or the patient could have renal failure and such. 05:26 Or what if the patient was drinking alcohol, as I gave you with the initial patient with the presentation? Please know that alcohol metabolites will compete with uric acid, so that uric acid can no longer be secreted into the urine. 05:40 Is that understood? Once again, let me repeat. 05:43 These alcohol metabolites are going to compete with uric acid so that uric acid can no longer be secreted. 05:50 So therefore, a patient is not able to excrete uric acid. 05:52 Welcome to Hyperuricemia, compliments of alcohol. 05:58 What kind of associations do you want to keep in mind? Well, chronic kidney disease, maybe hypertension, type 2 Diabetes, dyslipidemias. 06:04 You have a long little list. 06:06 Transplant patients, especially cardiac, related to cyclosporine. Keep that in mind. 06:10 All due to accumulation of what? The uric acid. 06:15 What's the cardinal signs of acute gout? It's a sudden onset of pain. 06:20 This pain, as I told you, is so, so severe that the affected joint, for example, the big toe, even if you were place a bed sheet, as light as it may be. 06:31 I don't mean a whopping comforter, and definitely not a brick, just saying a bed sheet. 06:36 A light, white bed sheet made out of cotton on that toe…ouch. That hurts. 06:44 That's the kind of pain we're talking about. 06:46 The joint is inflamed, inflammatory, red, hot, swollen. 06:50 Most common joint to be affected, the big toe. 06:52 It's called the metatarsophalangeal joint. 06:56 We call this podagra, right? Podagra.
About the Lecture
The lecture Crystalline Arthropathies: Gout / Pseudogout by Carlo Raj, MD is from the course Introduction and Non-Autoimmune Arthritis. It contains the following chapters:
- Crystalline Arthropathies
- Pathogenesis of Gout
Included Quiz Questions
A patient presents to the emergency department with excruciating pain in the 1st toe of his right foot which appears red and swollen. He has a history of similar episodes in the past. This condition is most likely the result of the deposition of which of the following crystals?
- Monosodium urate
- Phosphate
- Calcium
- Oxalate
- Potassium
Which of the following patients is most likely to present with gout due to overproduction of uric acid?
- A patient undergoing chemotherapy
- A patient with chronic renal failure
- A patient with nonalcoholic steatohepatitis
- A patient with a cardiac transplant
- An obese patient
What joint is most commonly involved in gout?
- 1st metatarsophalangeal joint
- 2nd metatarsophalangeal joint
- 1st metacarpophalangeal joint
- 1st distal interphalangeal joint
- 1st proximal interphalangeal joint
Which of the following medications is most strongly associated with hyperuricemia and gout?
- Cyclosporine
- Azathioprine
- Mycophenolic acid
- Methotrexate
- Tacrolimus
Customer reviews
1,0 of 5 stars
| 5 Stars |
|
0 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
3 |
3 customer reviews without text
3 user review without text