Playlist
Show Playlist
Hide Playlist
Coronary Vasculature and Conduction System of the Heart
-
Slides Structure-Function Relationships Cardiovascular System.pdf
-
Reference List Pathology.pdf
-
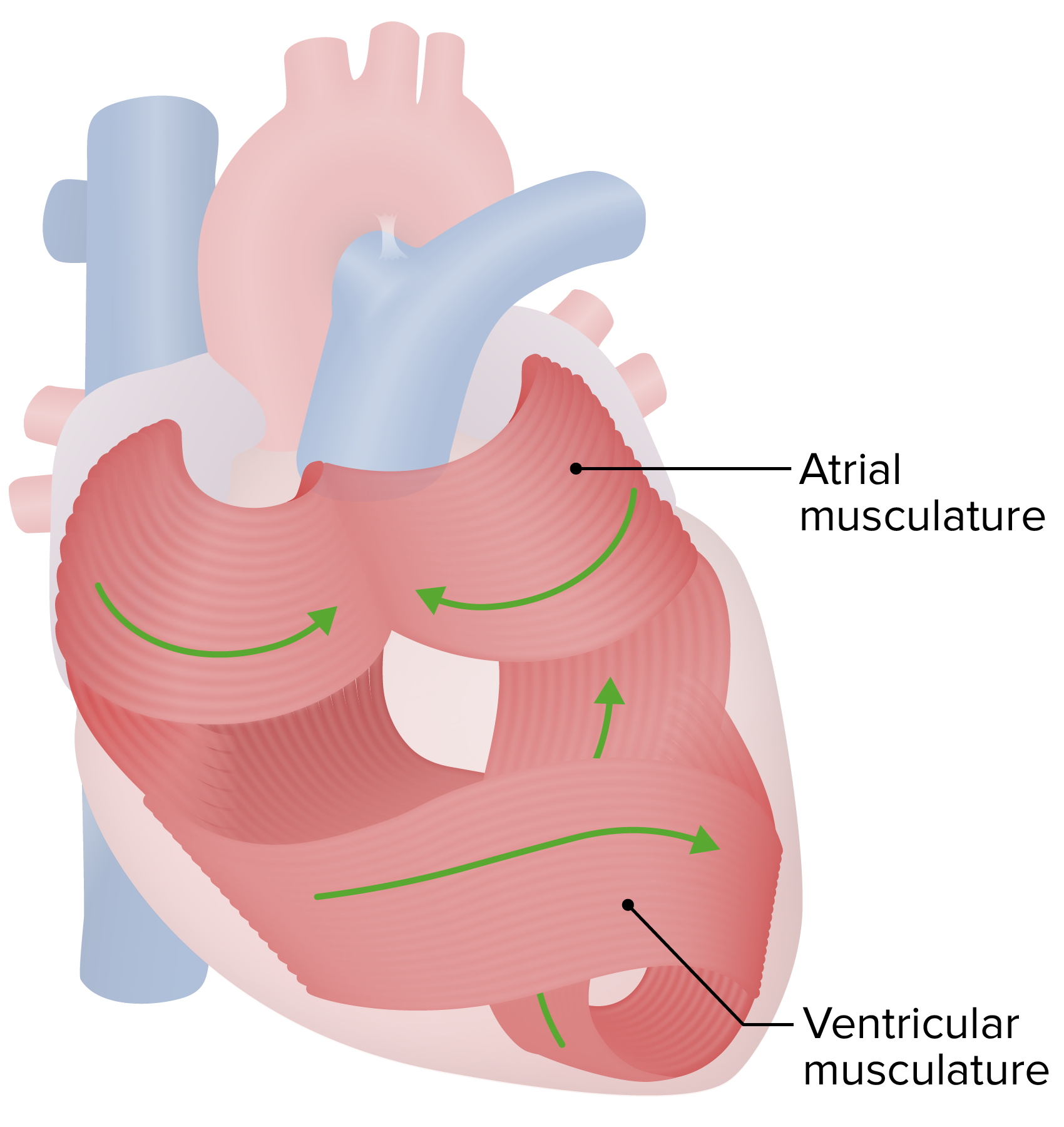
Download Lecture Overview
00:01 Okay. 00:02 Coronary vasculature. 00:05 So we've already talked about kind of the way that the vessels are laid out and how they get wrapped around the heart and perfuse different parts of the heart, we're going to just briefly review some of this. 00:16 Important point is that myocardial perfusion occurs during diastole. 00:21 As the heart is relaxing, when the heart is squeezing blood goes, whooshing by the coronary artery, take off the -- of the coronary arteries. 00:30 You're not getting any perfusion during systole. 00:33 It's only when the heart relaxes, the valve closes, and we get retrograde flow into those coronary arteries that we fill the heart. 00:41 So why do we care? Well, normally, during a normal heart cycle, when your systolic squeeze takes maybe a third of a second. 00:53 And if you're beating at 60 beats per minute, that means then you have two thirds of a second during diastole. 01:00 Now, let's double your heart rate to 120. 01:04 Now, you still have, it still takes that same third of a second to squeeze. 01:10 But now you have much less time, half the time, to fill during diastole. 01:16 So you can increase heart rates so much, that the heart no longer gets blood into the coronary arteries, and it can fail on that basis. 01:24 Ah, important point. 01:27 So this is just looking at when the vessels fill, and you can see that it happens when the aorta is going through diastole. 01:36 So when the aortic valve closes, that's when flow goes out the coronary vessels. 01:43 Okay, and finally to the conduction system. 01:45 And let's work our way down the basic structural elements of the conduction system. 01:50 So the pacer, the main pacer of the heart is the sinoatrial node. 01:55 It sits at the junction of the right atrial appendage and the superior vena cava. 01:59 So you can see that indicated there on the right. 02:02 It runs the heart, because it has the quickest release, the quickest loss of potential and then firing of any other cell type within the heart. 02:14 So in general, that's going to be where we have the regulation of how quickly the heartbeats. 02:20 There's clearly going to be hormonal, and neural inputs that also regulate how the sinoatrial node fires and how rapidly it fires. 02:32 Okay, we then once the sinoatrial node fires, we have to entrain the rest of the heart, we actually want the right atrium, the left atrium, to more or less squeeze in tandem. 02:44 So we have a Bachmann's bundle that goes from the sinoatrial node and carries the signal over to the left atrium and says, Dude, time for you to squeeze as well. 02:53 So that coordinates the atrial contractions. 02:56 There are some then ill-defined fibres that are responsible for getting from the sinoatrial node to the atrioventricular node, which sits pretty much near the fibrous septum between the atria. 03:08 That atrioventricular node holds the signal for just a little bit. 03:15 Why does it do that? It does that so the atrium can squeeze and fill the ventricle one last little bit about 15% of ventricular filling happens with that atrial kick. 03:26 So the AV node pauses for ever so short a period of time, allowing the atrium to contract, fill the extra 15%, into the ventricle, and then it sends the signal down to the rest of the heart, down to the apex of the heart through other fibers that we're going to talk about now. 03:43 So there are there's the bundle of His, which is indicated in green, and then there are the right and left bundle branches indicated as R and L, that get us quickly down to the apex. 03:54 All this connection system is modified cardiac muscle. 03:58 It's not nerve, it's modified cardiac muscle that is very quick and very efficient at transducing a signal down to the apex. 04:07 And then we get into the Purkinje fibres. 04:10 And this is the final kind of stage before we cause the initial depolarization of a cardiac myocyte. 04:18 Once any individual cardiac myocyte depolarizes. 04:21 It has a calcium transient increase that calcium goes between through gap junctions into the next cell. 04:28 It spikes, its contraction sends calcium into the next cell, in the next cell in the next cell, and we have this coordinated wave from the apex of the heart squeezing blood up and out. 04:38 Beautiful, beautiful! And with that we are concluded and I hope you have enjoyed thinking about how the heart is put together.
About the Lecture
The lecture Coronary Vasculature and Conduction System of the Heart by Richard Mitchell, MD, PhD is from the course Structure-Function Relationships in the Cardiovascular System.
Included Quiz Questions
When the heart rate increases, what will happen to the myocardial perfusion time?
- It will decrease because diastole decreases.
- It will increase because diastole increases.
- It will increase because diastole decreases.
- It will decrease because systole decreases.
- It will increase because systole increases.
Why is the sinoatrial node termed the “pacemaker of the heart”?
- It has the fastest action potential time.
- It delays the conduction signal to allow for atrial contraction.
- It is the only group of cells that is not regulated by neurohormonal elements.
- It sends signals in an uncoordinated fashion.
- If it is damaged, the heart will not beat.
What is true about the atrioventricular node?
- It delays the conduction signal to allow for atrial contraction.
- It delays the conduction signal to allow for ventricular contraction.
- It speeds up the conduction signal to allow for atrial contraction.
- It speeds up the conduction signal to allow for ventricular contraction.
- It is located near the interventricular septum.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |