Playlist
Show Playlist
Hide Playlist
Continuation of Case: 53-year-old Woman with Progressive Weakness and Balance Difficulty
-
Slides Diseases of the Spinal Cord.pdf
-
Download Lecture Overview
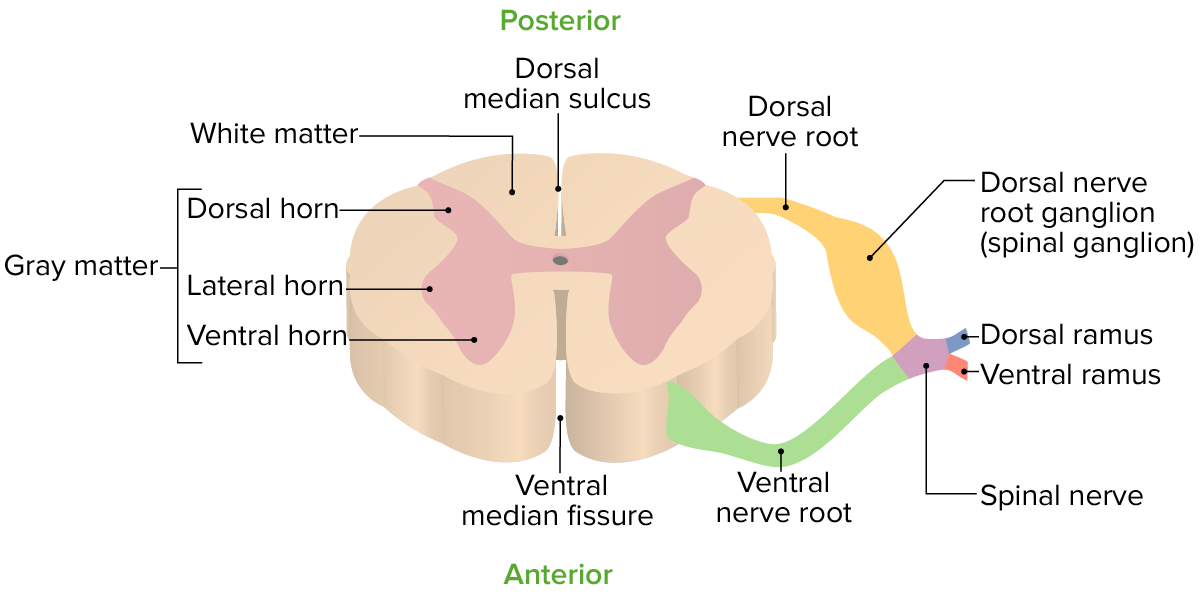
00:00 Now, let's talk about myelopathy from extradural pathology. And we're going to continue with our case of a patient who presented with slowly progressive paraparesis. 00:12 Initially developing in the legs and ultimately involving the hands that progressed over the course of about a year or even more. She began walking and then required a cane and walker and ultimately is in a wheelchair. By the time of her presentation to a neurologist, examination shows 4/5 strength in the bilateral lower extremities, 3+ deep tendon reflexes in the patella and Achilles bilaterally, and bilateral Babinski signs. This is the classic presentation of a myelopathy. Upper extremity examination showed 4/5 grip strength so she's weak in her hands, but normal proximal strength. 00:49 She is able to raise her arms. Normal deltoids, biceps, and triceps. There's atrophy in the hands bilaterally which tells us this has been going on for a while, this is not a sudden process. And fasciculations which is critically important. Fasciculations are lower motor neuron signs which tells us something's happening within the cell bodies of that cervical region of the spinal cord. There is also 1+ deep tendon reflexes in the bilateral upper extremities. So this is a typical presentation of someone with upper motor neuron signs in the legs and lower motor neuron signs in the arms. This could be spinal cord pathology and it could be motor neuron pathology. As we look and dissect some of the things that we see, again, we see 3+ deep tendon reflexes and Babinski signs in the lower extremities, upper motor neuron signs in the legs, and lower motor neuron signs in the arms with no crossover. And that's very important when we see the combination of upper and lower motor neuron signs in the same segment that points towards motor neuron pathology when we see this distribution. As we have in this case, that points to a spinal cord disorder. So this presentation is consistent with what type of myelopathy? Extradural, intradural extramedullary, or intradural intramedullary? Well, we said that those intradural intramedullary processes are things like multiple sclerosis, problems within the spinal cord and they often present with early bowel or bladder dysfunction with symptoms that involve the arms and then ultimately can involve the legs and we see the exact opposite of that in this patient. We see symptoms initially involving the legs and then working their way in towards the spinal cord, which is inconsistent with an intradural intramedullary process. This also is not suspicious for an intradural extramedullary process. For those, we think meningioma or peripheral nerve sheath tumors which often present asymmetrically, though pain is common in those patients, and we often have symptoms that are localized to one segment or area of the spinal cord which we don't see in this case. This is a pretty typical presentation of a patient who has an extradural process. Symptoms begin in the legs followed by arms, pain is common, and this should point towards a problem arising from the extradural space. So, what's going on and how do we approach the differential diagnosis and management of this patient? Well, here, localization is really helpful in driving our differential diagnosis. If we can conclude that this is an extradural process, there's only a handful of things that affect that area and the MRI of the spine is likely to be diagnostic of what's going on. And that's what happened for this patient. 03:40 Initially, the primary care physician ordered an MRI of the brain and as suspected it was normal. The problem isn't in the brain, the presentation is specific and really most focused on something in the spinal cord. Next, an MRI of the spine was ordered and you can see that here. If 2 cuts of the T2 image of the cervical spine and we see significant degenerative compression of the cervical spine. On the left, we can see areas of compression throughout multiple level C3, 4, 5, and 6. We see thickening of the posterior longitudinal ligament just behind their vertebral bodies, likely thickening of the ligamentum flavum just behind the spinal cord and in front of the spinous processes resulting in compression and narrowing of the spinal cord. If we look a little bit more closely, we can pick out 2 segments of the spinal cord. On the left, we're looking at something that's normal. This is an axial cross section of the spinal cord and we see the gray cord in the middle, white spinal fluid all the way around the cord telling us that it's healthy, but there is no compression, that the spinal cord looks normal in that area. As we come down to the area of degenerative compression, we see no spinal fluid around the cord. The cord has been flattened and compressed by thickening of the posterior longitudinal ligament. We no longer see the spinal fluid around the cord and that's really important for telling us that this is likely to be symptomatic compression of the spinal cord and this is the pathology for this patient. 05:16 Degenerative disease cervical spondylosis as the cause of this patient's presentation. 05:25 So, in our approach to non-traumatic myelopathy, MRI of the spine is critically important and here this patient's presentation and imaging points to an extradural process. Here, we're looking at cervical spondylosis and surgery is the mainstay of management for that patient.
About the Lecture
The lecture Continuation of Case: 53-year-old Woman with Progressive Weakness and Balance Difficulty by Roy Strowd, MD is from the course Diseases of the Spinal Cord.
Included Quiz Questions
Which of these is a sign of extradural myelopathy due to degenerative cervical spondylosis?
- Hyperreflexia in both lower extremities
- Fasciculations in the lower extremities
- Negative Babinski sign (downgoing toes) bilaterally
- Flaccid paralysis in the legs
- Atrophy in the feet
What is the mainstay of management for a mass causing extradural compression?
- Surgery
- Glucocorticoids
- Opioid analgesics
- Chemotherapy
- Radiation therapy
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |