Playlist
Show Playlist
Hide Playlist
Clinical Manifestations and Management – Pericarditis
-
Slides Myocarditis Pericarditis.pdf
-
Reference List Pathology.pdf
-
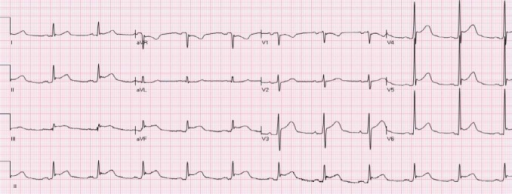
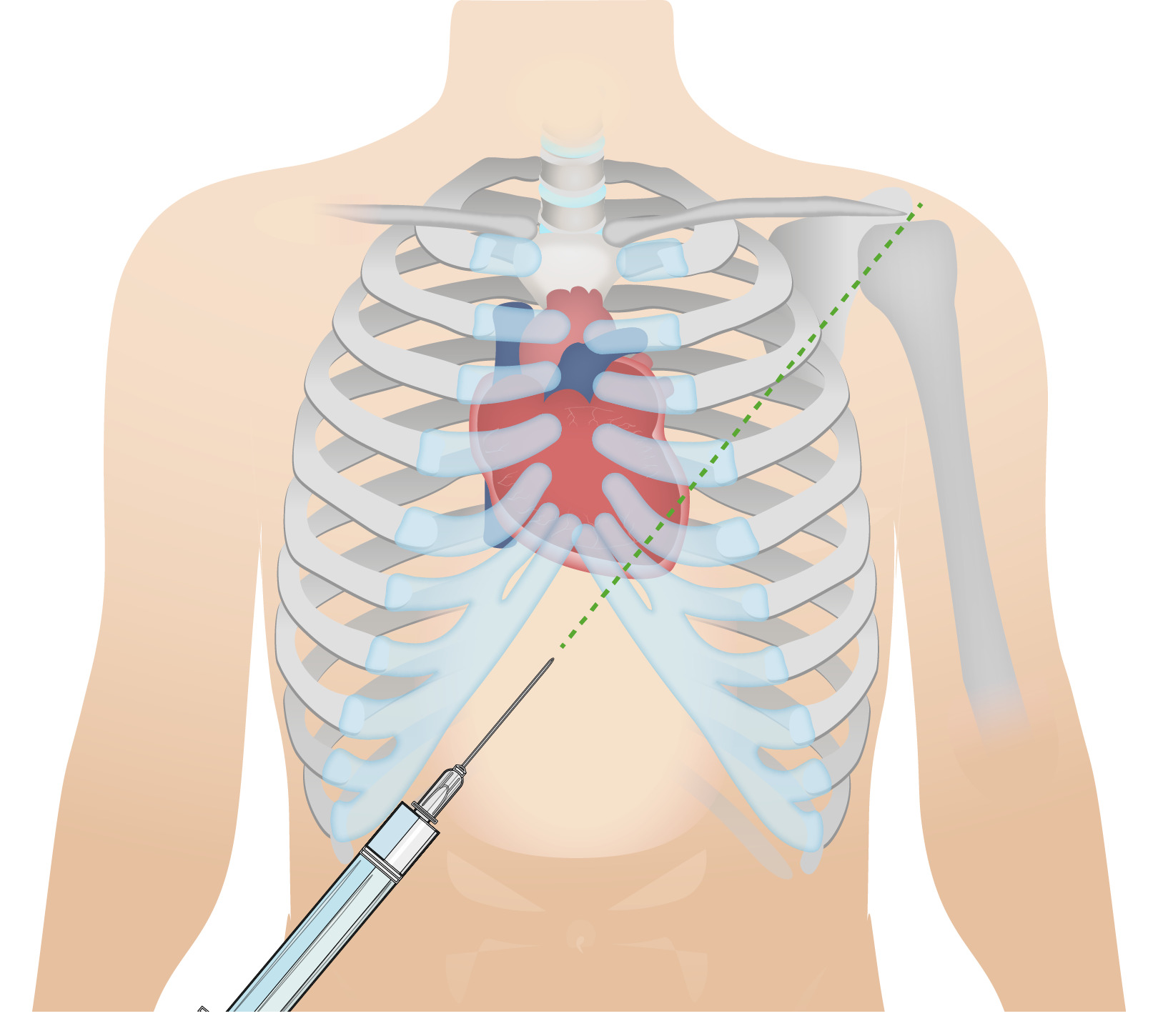
Download Lecture Overview
00:00 So, acute pericarditis, what are the signs and symptoms? How do you recognize this in your patients? Because it is acute inflammatory, there will be a fever. Okay, that’s fine. 00:10 There’s also often a very sharp pleuritic and positionally dependent pain. So, pleuritic means it gets worse when you take a deep breath. Well, that’s because you’re rubbing the lung up and down or moving the pericardium up and down and that’s aggravating nerve fibers so you feel pain, and that’s why it’s also dependent and positional. 00:30 And certain positions will make it go away as you get the heart away from the pericardial lining. There will also be a pericardial friction rub, meaning you put in your stethoscope and you hear something that sounds like sandpaper. As the heart is beating, it’s moving within the pericardial sac and if there’s inflammation or fibrin or anything else in that space, it’s kind of rubbing, so it’s really kind of like sandpaper. 00:52 It’s also why it hurts, it’s a very sharp pain. Frequently, patients will say it gets better as I move forward and as the heart kind of moving dependently in that position and frequently the pericarditis will be posterior, won’t be uniformly involving the heart but will be posterior if I move the heart away from that inflamed posterior pericardium it may improve. Because we are causing a restrictive physiology and we have diastolic dysfunction, we will see signs associated with that such as elevated jugular venous pressure and you will see an elevated jugular venous distention, again indicating that the heart is not able to fill appropriately and we’re getting back accumulation of fluid here in the venous circulation. As part and parcel of that same constrictive physiology, we’re going to get peripheral edema, again because we are getting venous return that is not able to be pumped through the heart because we don’t get good diastolic filling. Patients not only have right-sided symptoms of heart failure due to constriction but can also have left-sided symptoms, so they will be dyspneic. They will have fluid pressure backing up into the pulmonary circulation, so they will be short of breath. 02:14 They frequently also will have tachycardia. This is because the heart is not able to fill appropriately and so the cardiac output is diminished. To compensate for that, the patient has a greater heartbeat at greater rate to maintain cardiac output. 02:30 And the nature of the accumulated fluid within the pericardial space will cause pulsus paradoxus. Pulsus paradoxus occurs when there is a big difference between the systolic pressure and diastolic pressure as a function of the respiratory cycle. 02:46 And the greater that is, normally it should only be 30 or 40 mmHg between systole and diastole and as that changes or increases during the respiratory cycle, that's pulsus paradoxus and happens as a part of chronic pericarditis. When we look at the ECG, we see that there are nonspecific ST segment elevations, suggesting that there is some variation in repolarization. How do we manage this? Well, for a lot of the forms, fortunately, if we just give a little bit of anti-inflammatories such as high-dose aspirin, nonsteroidal anti-inflammatories maybe just a little bit of analgesia and some oxygen, the patients will self-resolve and we’re good to go. In more severe cases, particularly with a constrictive pericarditis end stage, very little you can do for that other than to open up or remove the pericardial sac. With that, we very quickly have gone through various pericardial diseases.
About the Lecture
The lecture Clinical Manifestations and Management – Pericarditis by Richard Mitchell, MD, PhD is from the course Myocarditis and Pericarditis.
Included Quiz Questions
What movement classically improves the symptoms of pericarditis?
- Leaning forward
- Standing
- Deep breathing
- Walking
- Lying down
What finding is seen in the vast majority of patients with acute pericarditis?
- Pleuritic chest pain
- Nausea and vomiting
- Positive antinuclear antibody
- Dull epigastric pain
- Fever and chills
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |