Playlist
Show Playlist
Hide Playlist
Classification and Causes of Vitamin B12 Deficiencies
-
Slides Macrocytic Deficiency.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
00:02 Now with B12 deficiency, let’s go from head to toe. 00:05 Okay, head to toe. 00:05 All the different ways your patient is going to become B12 deficient. 00:09 Forevermore, forevermore, separate your pernicious anemia from all of the other causes of B12 deficiency. 00:17 So those of you that are only thinking about pernicious anemia, you know that’s not right. 00:21 So B12 deficiency maybe, maybe your patient is a vegan. 00:27 Remember, in industrialized and developed countries, very difficult to find a patient that has not had proper B12 consumption; dairy, meat, so on and so forth. 00:39 And also, how long do you store B12 in the liver? Seven years at least, that’s a long time. 00:44 So very difficult for a patient to be B12 deficient in a developed country. 00:49 Okay. 00:51 So in a developed country, then you might be looking for a patient who's in a vegan diet, right? Not vegetarian but vegan to the point where they are not even consuming enough of your B12. 01:01 That’s a possibility. 01:04 So what happens here? You’re worried about breast fed infants of pure vegans also. 01:09 Important there in terms of possibly a child or infant being B12 deficient. 01:12 In addition, same thing, you’re not taking up enough B12, but malnutrition, but in a nursing home, it’s always difficult. 01:20 in a nursing home it’s always difficult. 01:20 You’ll never know if the elderly are receiving proper care, right? So they could be malnourished for many things, maybe folate deficiency, maybe iron deficiency, maybe B12 deficiency, but for years. 01:33 Is that clear? Obviously, this has nothing to do with pernicious anemia. 01:36 Let's continue. 01:38 Malabsorption: Now, take a look at my discussion. 01:40 Autoimmune destruction of parietal cells. 01:42 So what is this? Good. 01:45 This is pernicious anemia. 01:46 So autoimmune destruction. 01:49 Think of where you are. 01:51 Fundus. 01:52 Body. 01:54 Proximal portion. 01:54 Parietal cells. 01:57 Think about the receptors that stimulate acid, right? So your CCK A and B receptors with your gastrin. 02:02 You have another one called H2 receptors. 02:04 And you have another one called M3. 02:07 Can you picture all that? All that stuff we talked about in physio, biochem and so forth. 02:13 If you knocked out the parietal cell, then you have no acid. 02:16 And you also have no intrinsic factor and that’s a problem. 02:20 So if there is no intrinsic factor, I have lost a chaperone for B12. 02:25 And so for all intent and purposes, you are B12 deficient. 02:27 From henceforth, I would like for you to keep pernicious anemia separate from all others. 02:33 In gastroenterology, would you tell me what autoimmune of destruction parietal cell -- what kind of chronic atrophic gastritis that is? Take the A in autoimmune and that will tell you what it is. 02:45 This is gastric type or the fundic type of gastritis. 02:50 This will be type A, right? Type A, if you remember. 02:53 So in gastroenterology, the type of atrophic gastritis, this is called type A. 02:58 Take a look at the A and that will help you. 03:00 You separate the cell. 03:01 Tell me about the acid level in your stomach. 03:02 What do you call that clinically? Good. 03:04 Achlorhydria. 03:06 What does A- mean? Without. 03:08 What does chlor- mean? Tell me what that acid in the stomach is made up of. 03:12 Hydrochloric acid. 03:15 So if there is no acid, it’s achloric acid. 03:18 Fantastic. 03:20 Stop. 03:21 Give me few other issues in the stomach? We have to, I’m so sorry, we have to. 03:25 Because you can’t just memorize this. 03:29 If you don’t have enough acid, can you properly convert your methemoglobin into ferrous? Meaning can you convert your ferric into ferrous? No. 03:36 So at the same time, could you also be iron deficient? Yes. 03:39 We talked about that. 03:41 Now, be careful though because one other thing, real quick. 03:45 Remember that acid in the stomach, physiologically would you tell me as to what the peptide is coming out of your chief cell in your stomach? Good. 03:53 Pepsinogen, right? And how do you clear off that -ogen? Oh, the acid, yeah. 04:01 So if you don’t have acid, you can’t form proper pepsin. 04:04 And tell me what food type is not being properly digested? Is it protein? Is it carbohydrate? Or is it lipid? Peptide. 04:11 Good, protein. 04:13 Interesting, huh? Play around with this and make sure you know it well. 04:16 So far, we've talked about the diet. 04:19 Then we went into what’s known as the, well, stomach. 04:24 Let’s move on. 04:24 Decreased gastric acid, we talked about pepsinogen and intestinal reabsorption. 04:30 What’s going on here with malabsorption? Maybe your patient has eaten, let’s say there is a wheat bread or rye bread or some sort, and has issues with malabsorption. 04:41 Celiac, of course. 04:41 Celiac is what we're -- Gluten, gluten. 04:45 And so with gluten, that could be a problem, endomysial and transglutaminase. 04:50 We talked about that in gastroenterology. 04:54 So intestinal reabsorption, celiac. 04:57 Number two, Crohn’s disease. 04:59 In Crohn’s disease, from head to toe, it can affect you anywhere. 05:03 Head to toe by the way, most commonly the terminal ileum. 05:08 That’s important, isn’t it? Tell me about the terminal ileum and where the B12 functions? B12 gets reabsorbed in the intestine in the terminal ileum. 05:16 So if Crohn’s disease which is an inflammatory bowel disease is not functioning -- you’ve heard of cobblestone appearance, skip lesions, then you can’t take up B12. 05:25 So Crohn’s and celiac. 05:26 Bacterial overgrowth, that’s important. 05:28 I’ll tell you later. 05:29 Give me that fish tapeworm. 05:30 For example, there is a scenario in which the son went out with the grandfather and they went fishing in the Great Lakes by Michigan. 05:41 So let it be Lake Michigan, Lake Huron, Lake Ontario, whatever it may be, Lake Erie. 05:46 And they then fished and they caught trout and after catching trout all of a sudden -- not all of a sudden, but now there is a development of megaloblastic anemia. 05:55 What’s the name of that fish tapeworm? That crazy name -- I don't know. I mean, you could probably pronounce it better than I can, Diphyllobothrium latum, right? It’s a crazy fish tapeworm that preferentially likes to consume B12. 06:08 Fantastic! Where did you get it from? The fish, trout. 06:12 Where? Usually on the great lakes. 06:14 So think about, you know, Michigan. 06:17 Think about maybe the Western portion of Pennsylvania. 06:20 Think about those areas, Illinois, so on and so forth. 06:24 And chronic pancreatitis. 06:26 This is important as well. 06:29 You will see why. 06:29 So, you’ve taken B12, maybe from dairy, maybe from meat. 06:34 You’re chewing it and between the mouth and the stomach, you’re going to pick up another chaperone. 06:42 It’s called R-factor. 06:42 Remember this one? Don't forget this one, R-factor. 06:46 What was that other chaperone with B12? That was intrinsic factor. 06:48 You must know both. 06:51 If it’s lack of intrinsic factor, what’s your diagnosis? Pernicious anemia. 06:56 If it’s pancreatitis, why do you need the pancreas here for proper B12 metabolism? You need the pancreas to remove the R-factor. 07:03 And if you don’t remove the R-factor for all intent and purposes, you are B12 deficient. 07:08 So if a patient has chronic pancreatitis, for example, what’s the most common cause of pancreatitis in a child? Cystic fibrosis. 07:16 Most common cause of pancreatitis in an adult? Alcohol. 07:20 If an individual has pancreatitis and you see megaloblastic anemia, vitamin B12 deficiency may be present. 07:26 Next, increased utilization, pregnancy/lactation, absolutely. 07:31 You know, once again, we talked about more so deficiency in the pure vegan. 07:37 Okay, ladies and gentlemen, a table extremely important. 07:41 There is no way you should be memorizing this. 07:42 These discussions we've had in many different organ systems, bringing a little bit of physiology but it’s purely dealing with B12 deficiency. 07:51 What you want to do is separate your pernicious anemia from all other causes of B12 deficiency. 07:58 You tell, which one of these B12 deficiencies only presents with achlorhydria? Good. 08:06 Pernicious anemia.
About the Lecture
The lecture Classification and Causes of Vitamin B12 Deficiencies by Carlo Raj, MD is from the course Macrocytic Anemia – Red Blood Cell Pathology (RBC).
Included Quiz Questions
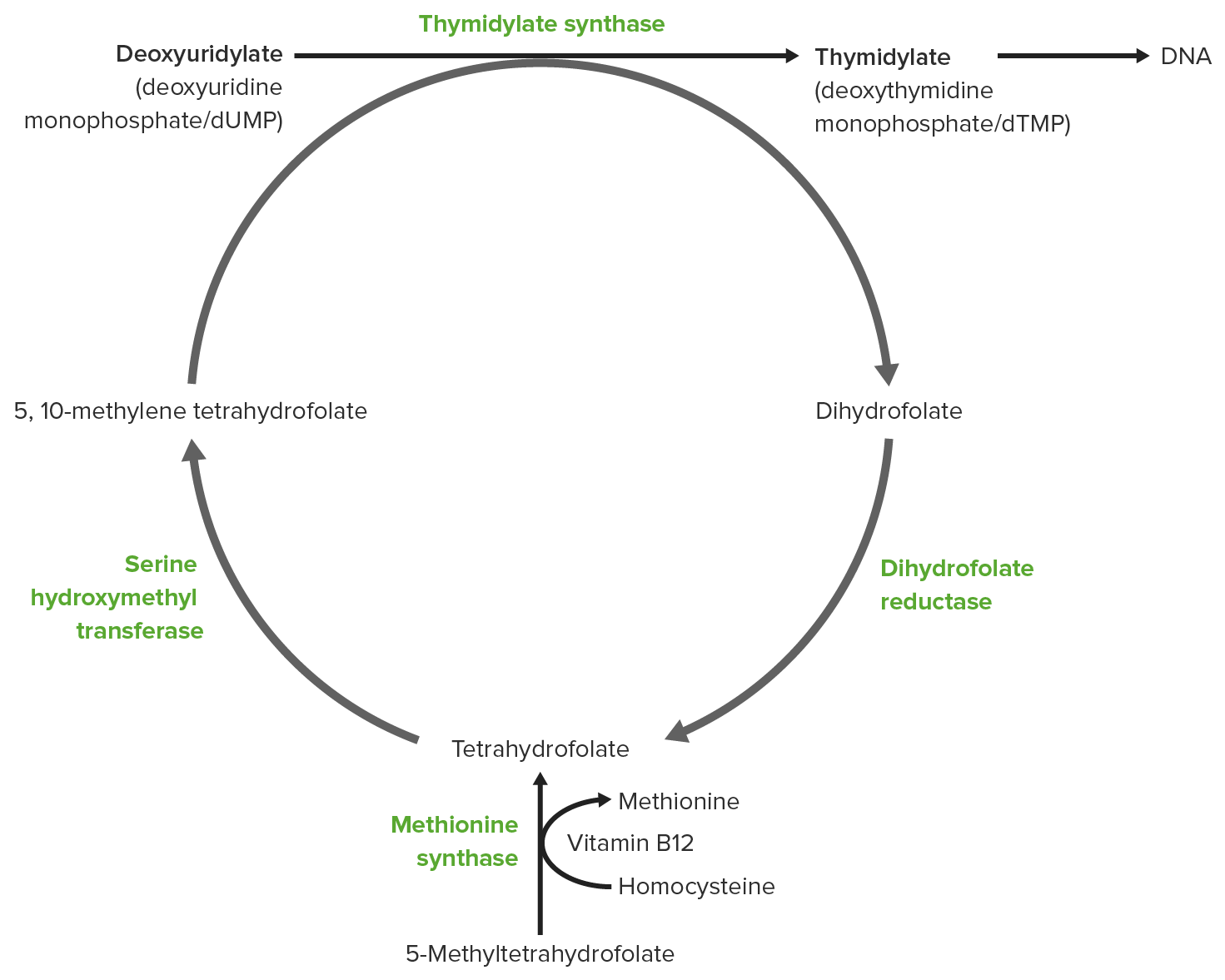
Which of the following contributes as an intermediate carrier of the methyl group from methyl-tetrahydrofolate to homocysteine?
- Vitamin B12
- Vitamin B6
- Ornithine Transcarbamylase
- Dihydrofolate
- Uridine monophosphate synthetase
What is a common etiology of decreased intrinsic factor leading to vitamin B12 deficiency?
- Autoimmune destruction of parietal cells
- Iron deficiency anemia
- Lactase enzyme deficiency
- Chronic use of NSAIDs causing gastritis
- Small intestinal bacterial overgrowth
What enzyme is inhibited by methotrexate, leading to megaloblastic anemia?
- Dihydrofolate reductase
- Thymidylate synthase
- Phosphoribosyl pyrophosphate (PRPP) synthase
- Ribonucleotide reductase
- Uridine monophosphate synthase
Which of the following, when damaged, most likely leads to loss of proprioception in B12 deficient patients?
- Dorsal column
- Lissauer’s tract
- Spinocerebellar tract
- Corticospinal tract
- Anterolateral tract
Autoimmune destruction of which of the following cells can cause megaloblastic anemia?
- Parietal cells
- Secretin cells
- K cells
- I cells
- Chief cells
Which of the following becomes deficient following the autoimmune destruction of parietal cells?
- Intrinsic factor
- Somatostatin
- Secretin
- Cholecystokinin
- R binder protein
In patients with Crohn's disease, involvement of which part of the gastrointestinal tract is most likely to cause megaloblastic anemia?
- Terminal ileum
- Jejunum
- Pylorus
- Antrum
- Duodenum
Vitamin B12 deficiency is most likely with prolonged infection with which of the following organisms?
- Diphyllobothrium latum
- Clonorchis sinensis
- Necator americanus
- Echinococcus granulosus
- Schistosoma mansoni
Which is the following conditions is most likely to cause vitamin B12 deficiency and achlorhydria?
- Pernicious anemia
- Crohn’s disease
- Malnutrition
- Alcoholism
- Chronic pancreatitis
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Excellent nice little concept explanation on an important topic for USMLE