Playlist
Show Playlist
Hide Playlist
Changes in Glomerular Dynamics 1
-
Slides RenalBloodFlow1 RenalPathology.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
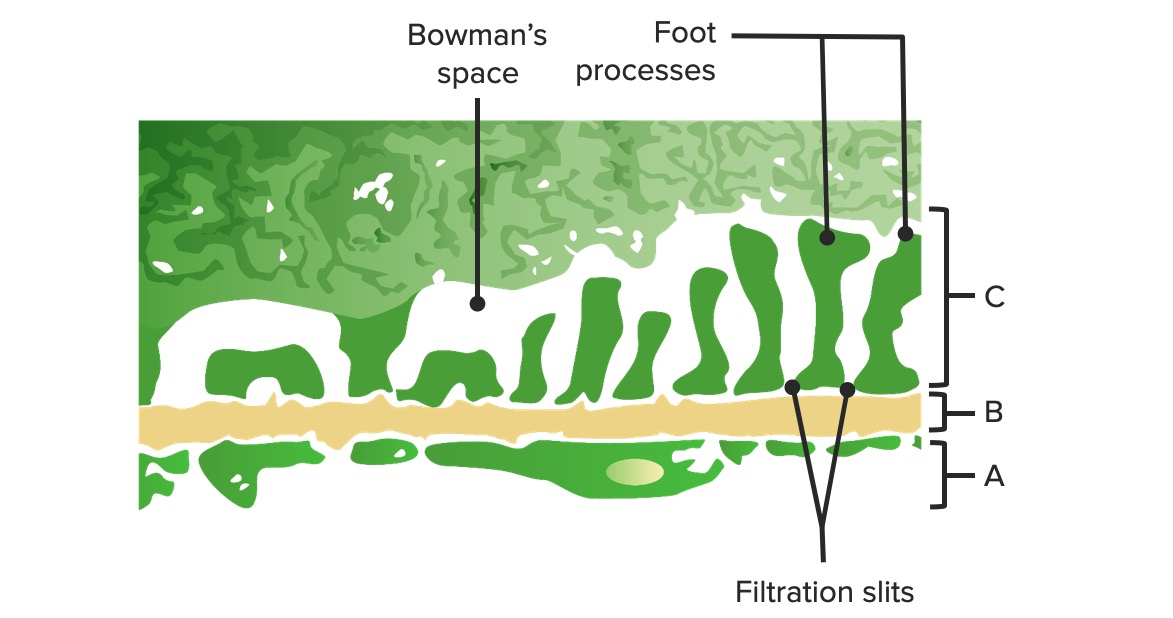
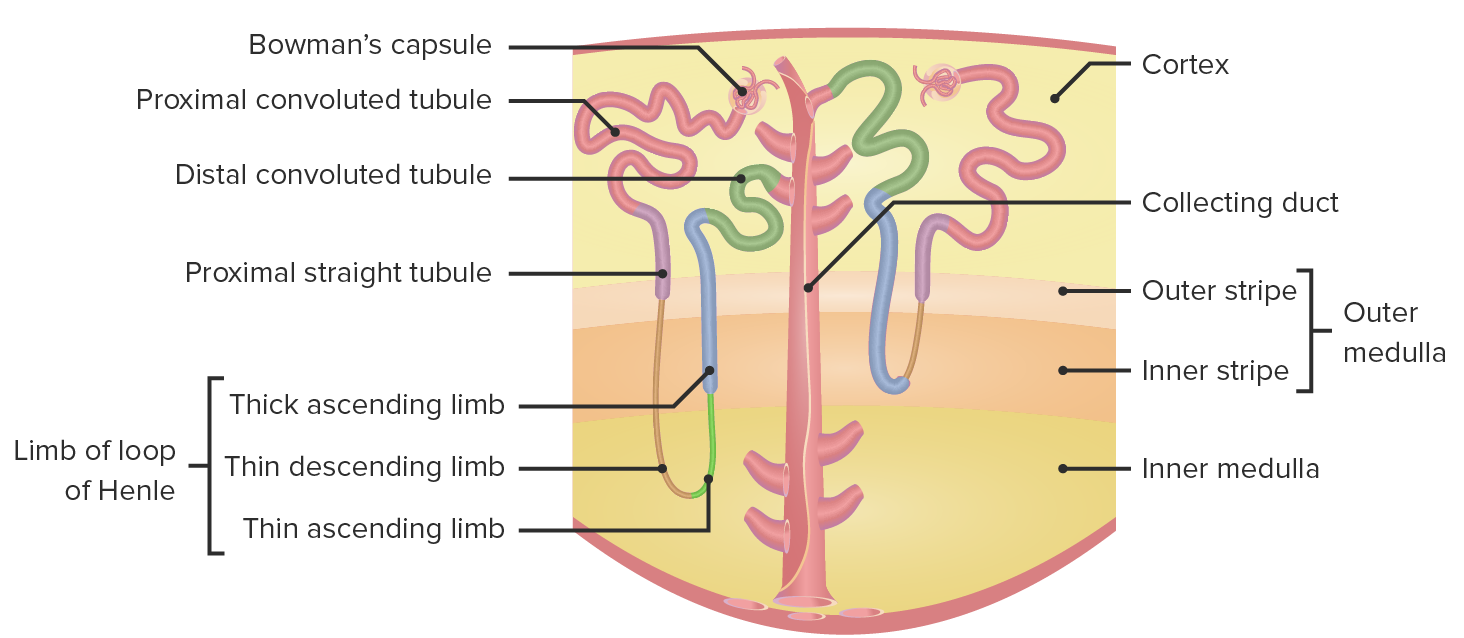
00:00 Now, an important table. I love this because here’s my table. Oh, really? Here’s your table. 00:07 And then, there’s your clinical applications. I’m going to show you how to read this, so you’re not just sitting there and memorizing because you don’t have time to do that. 00:15 What you do have time is to understand so that you don't have to keep coming back, keep coming back, keep coming back. What did he say? What did he say? What did he say? No. 00:21 You’ll learn it. Well, the first, maybe one. Come back, second time. You keep adding this information. 00:27 Before you know it, it’ll be a permanent part of your history, really it will be. Okay? Watch this. 00:33 So let’s begin with our picture. We have a tube coming in from the top. It’s your afferent arteriole. 00:40 I want you to pay attention towards this Bowman's space, okay? Now, in that Bowman's space, think about what should be happening, plasma being filtered, plasma being filtered. 00:52 What is passing through your afferent arteriole and the tuft of capillaries. It is the fluid, “the water” the electrolytes, sodium, potassium, chloride, bicarb, amino acids, such. Protein? No, no, no. 01:06 Albumin should never pass through there. Never. Okay? So it’s very, very restricted or limited in terms of what it’s filtering. That point there, it says Bowman’s hydrostatic pressure. 01:19 Should there be increased hydrostatic pressure in the Bowman's space? Listen to my question. 01:26 Should there be hydrostatic pressure in the Bowman's space? No. It doesn’t make any sense. 01:35 Should there be hydrostatic pressure in the glomerular capillaries? Yes. Seeing this right now? Not quite yet? Hold on. What if there was hydrostatic pressure in the Bowman’s space? You automatically think pathology. Period. What pathology? Obstruction. Where? Listen to this patient. Are you ready? 72-year-old male, old, okay? Probably want to, don't tell him what you want, tell him that but anyhow, elderly shall we say? And the 72-year-old has to go to the bathroom, has to go to the bathroom, has to go to the bathroom. 02:13 Everytime he goes to the bathroom or frequently, he’s not able to properly void. Tell me diagnosis. 02:18 BPH, Good, benign prostatic hyperplasia. Is that an obstruction? Yeah. What is that obstructing? The urethra. Are you there? It’s obstructing the urethra. What is it doing? But Doc Raj, this is the glomerulus. You’re obstructing urethra? Of course. Come on now. 02:36 So you are obstructing urethra. Back up now. Back up into where? Urinary bladder. 02:42 Back up more. Ureter. Hydronephrosis. Back up where? Glomerulus. What happens to hydrostatic pressure? In the Bowman’s space, it’s increased. Welcome to pathology. 02:52 Do you understand how to read this now? So Bowman’s space, hydrostatic pressure should never be present or should not be significant. And if you have some type of obstruction, you’re going to increase that hydrostatic pressure, point number one. Now, what we’ll do is I’m going to identify the different components here and put in the appropriate pathologies. 03:14 And in the table, I’m going to show you something that’s really important for you. 03:18 Yeah, but give me a moment. I want us to come down here now. Let's start once again. 03:24 But this time, we’ll talk about oncotic pressure. What’s oncotic pressure mean to you? And I'm assuming from physio, you’re strong in your Starling forces. If you’re not, well, just make sure that we repeat. Hydrostatic pressure? Pushing pressure. Oncotic pressure? Pulling pressure. By pulling I mean P-U-L-L-I-N-G, literally pulling. Okay. What does oncotic pressure mean to you? It means protein. My question now to you is Bowman's space. 03:53 I’d just gotten to telling you that the GFR and the tuft of capillaries is filtering what? Plasma, electrolytes, maybe small proteins, but definitely not albumin. 04:06 So for all intent and purposes, would you tell me clinically the actual Bowman’s space oncotic pressure significance? Is it significant or no? Oncotic pressure. No. 04:19 There shouldn’t be any albumin there. The Bowman's space has basically zipped oncotic pressure. 04:24 It shouldn’t. What if you did present with oncotic pressure in Bowman’s space? Give me diagnosis. 04:30 Nephrotic syndrome. Period. Nephrotic syndrome. Maybe nephritic. But what if it was a child? If it was a child and was urinating quite a bit, and the urine was foamy perhaps, and the child was also developing edema, and had hyperlipidemia, give me diagnosis. 04:47 MCD, minimal change disease. There you have it. The most common cause of nephrotic syndrome in a child. Point number two, are you getting the hang of this now? Let’s move on to number three. 05:00 Now, with number three, I’m going to move into our table here so that we can get into more of a flow and keep things relevant. But those were two huge points within the Bowman’s space. 05:10 I’m going to start with just the top of the table here with constriction of ureter. 05:14 You’re going to help me figure out the labs. You’ve seen the picture already. 05:19 We just want to make sure that you’re clear about how to interpret things. 05:24 Start with the beginning, constriction of ureter. Close your eyes. Where are you? Ureter. Distal to the kidney. Constriction of ureter. How did that occur? Maybe renal stone. 05:34 Well, maybe perhaps even that BPH patient in which what happened, there was obstruction. 05:40 So I don’t care. Point is something beyond the kidney was providing obstruction. 05:46 Okay. Now, what happens? Tell me about renal plasma flow. No change. NC stands for no change. 05:54 How could there be any change in the renal plasma flow when the obstruction is the ureter and company? No change. Now, why is GFR decreased with constriction of the ureter? It comes back to understanding that picture that we saw with what? Obstruction and increased hydrostatic pressure in the Bowman’s space. If you increased, close your eyes, think about this. 06:19 If you have increased hydrostatic pressure in the Bowman’s space, what happens to GFR? You’re pushing and preventing filtration from taking place. We have a decrease in GFR. 06:31 Stop there. Please stop there because here, what you'll have to memorize is filtration fraction. 06:39 Normal filtration fraction is approximately 20%. That you know from physio. All I’m trying to do here is lay down the concepts. So filtration fraction is equal to GRF over RPF. 06:52 Go in alphabetical order: G-glomerular filtration rate, R-renal plasma flow. You tell me, which is the only parameter that was affected here with constriction? Good. GFR. 07:09 If you only decrease the numerator and the RPF, renal plasma flow, which is denominator, which is constant, now this, I can’t help you with. This is just simple math. Okay, really. 07:19 If all that you’re doing is decreasing numerator, what happens to ratio? It decreases. 07:25 Welcome to filtration fraction decreasing with obstruction. Let’s move on to the next one. 07:30 This is your patient with decreased plasma protein concentration. Listen to what that is saying. 07:38 So now you’re tired. Okay? It’s been a long day. Maybe you’ve been listening to me for a long time. 07:43 Maybe you’re doing a rotation. You’re doing your internship. You’re taking your board exams. 07:47 It’s been a long day. You are tired. Is that any excuse to get things wrong? No, it’s not. 07:53 So work with me here. Okay? You with me? All right. Decreased plasma protein concentration. 07:59 What does that mean? That means that albumin and company is leaving the plasma, going into the Bowman’s space. Oh, boy! What is this? Well, I gave an example of minimal change disease. But Dr. Raj, you told me that Bowman’s space, oncotic pressure was increasing. Correct. Why? Because the protein was leaking out of the plasma into the Bowman's space. Do you see the differential or do you see the difference? Now, you work with me here once again. Tell me about renal plasma flow. It’s not affected. 08:31 No change because you’re losing protein. Next, what happens to GFR? Unfortunately, it’s actually increased. Tell me about your patient with nephrotic syndrome. Wow! Greater than three and a half grams of protein per day that’s being lost. In addition, there’s lots of urine. So, this is pathology. The fact that you’re losing more GFR in this type of setting, not a good thing. What do you think happens to filtration fraction? Obviously, increased. Why? The only thing that you’re increasing is GFR. Let's ove on. We have afferent arteriole constriction. 09:03 What happened here? Afferent arteriole constriction maybe, just maybe, your patient was taking NSAIDs. Dr. Raj, I don’t know how to do this. Yes, you do. Are you ready? Afferent arteriole. Why NSAIDs, nonsteroidal anti-inflammatory drug? What does that mean to you? Well, we have prostaglandins. What do you know about NSAIDs? It’s a COX inhibitor. 09:26 It’s cyclooxygenase. And so, that's an enzyme that’s being inhibited by NSAID, right? And so therefore, what are you inhibiting the production of? Prostaglandins. What does that mean? Normally, what kind of effect does prostaglandin have on the afferent arteriole? Do you remember this? Yeah. If you don’t, know it now. Prostaglandin, wherever it is, is always going to bring about vasodilation, especially prostaglandin E. So prostaglandin E will cause vasodilation of the afferent arteriole. What's my topic? Afferent arteriole constriction. 10:01 How can you remove the prostaglandin therapeutically and medically? It’s called NSAIDs. 10:07 In the US, we have ibuprofen, maybe we have Motrin, okay? You all probably know about aspirin. 10:14 So if you knock out the prostaglandin, why would this patient be taking NSAIDs? My goodness! How prevalent is arthritis? Quite. How long do you think this patient might be taking NSAIDs? I don’t mean just days and weeks. I’m talking years, 10, 15 years. And you knock out that prostaglandin? Not a good thing. It’ll cause afferent arteriole constriction. Not a good thing. 10:36 So what happens to renal plasma flow? It’s stopped or it’s slowed down, decreased. What about GFR? A decreased amount of blood passing through afferent, so therefore, decreased GFR. 10:47 What about filtration fraction? No change. Are you seeing the integration process here? Pathology, pharmacology, physio, all must be put together. Let’s continue. Efferent arteriole, what about this one? Efferent arteriole constriction. You tell me what hormone on the efferent side would cause constriction? It’s called angiotensin II. Do you remember that from physio? And so, what I’m saying obviously is the fact that your foundation has to be strong so we can move through this quickly. Angiotensin II preferentially has effect to an efferent. What does it want to do? It causes vasoconstriction. When it does so, what kind of effect will it have on your renal plasma flow? It doesn’t have. Well, it slows it down. 11:29 And it causes vasoconstriction and it slows it down, number one. Number two, well, if you constrict your efferent arteriole, what then happens to your GFR? It’s increased. Why? Close your eyes. 11:42 Where am I? Efferent arteriole. Take a look at the picture. Efferent. If you constrict it, what then happens proximally? Increased hydrostatic pressure, increased GFR. 11:52 Now, you put all these together, filtration fraction. And GFR over RPF, do a simple math. 12:00 You’re moving in opposite direction, GFR increasing, RPF decreasing, overall, filtration fraction increasing.
About the Lecture
The lecture Changes in Glomerular Dynamics 1 by Carlo Raj, MD is from the course Renal Diagnostics.
Included Quiz Questions
Which of the following does not occur in response to a pathological constriction in the ureter?
- Increase in the renal plasma flow.
- Decrease in the filtration fraction.
- Decrease in the glomerular filtration rate.
- Increase in the hydrostatic pressure in Bowman’s space.
What is the normal filtration fraction of the kidney?
- 20%
- 10%
- 40%
- 25%
- 15%
Which of the following changes would occur in a patient with nephrotic syndrome?
- Increase in the oncotic pressure in Bowman’s space.
- Decrease in the hydrostatic pressure in the glomerulus.
- Increase in the plasma protein concentration.
- Decrease in the GFR.
- Decrease in the filtration fraction.
Which of the following describes the mechanism of action of angiotensin II in the kidney?
- Constriction of the efferent arteriole.
- Constriction of the afferent arteriole.
- Vasodilation of the efferent arteriole.
- Inhibition of prostaglandin production.
- Increase in the oncotic pressure.
Which of the following changes would NOT occur in the kidney in response to the long-term administration of NSAIDs?
- Decrease in the filtration fraction.
- Inhibition of prostaglandin E.
- Decrease in the glomerular filtration rate.
- Constriction of the afferent arteriole.
- Decrease in the renal plasma flow.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |