Playlist
Show Playlist
Hide Playlist
Cerebritis and Brain Abscess
-
Slides CNS Infections Cerebritis.pdf
-
Download Lecture Overview
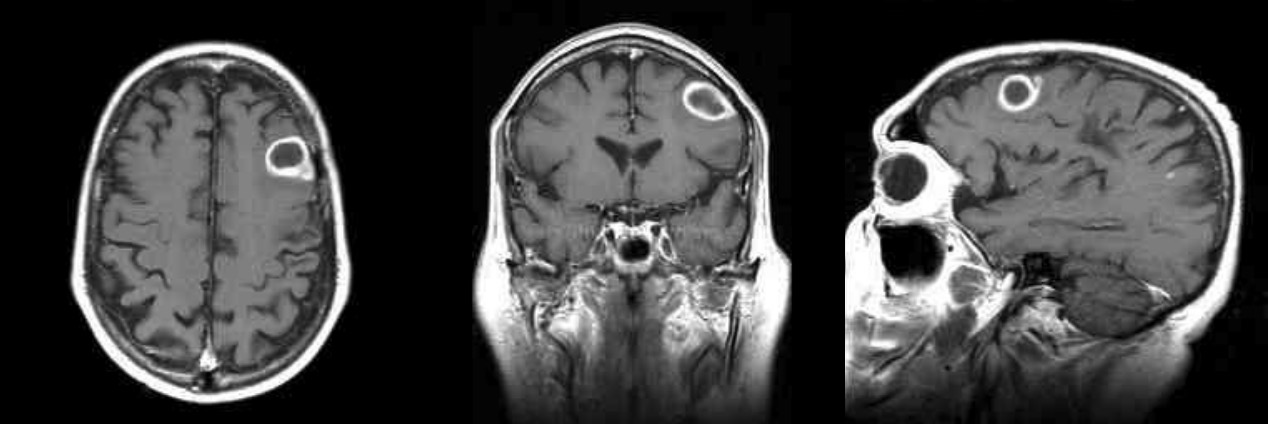
00:00 So, let's learn about cerebritis and brain abscess. What are those terms? Well unlike meningitis which is infection on the outer surface of the brain, the dura mater, or encephalitis which is a global neurologic dysfunction and infection in the arachnoid, subarachnoid and pia mater, cerebritis and brain abscess are infections that occur within the brain parenchyma. We're talking about focal suppurative infections within the brain, the brain tissue, the brain parenchyma. And this can vary on a spectrum, from cerebritis which is poorly demarcated, you can't draw a line around it to abscess which you can draw a line around. And an abscess is typically an area of focal walled-off infection that's surrounded by a vascular capsule and that means abscess. This is uncommon, it's the least common of the 3 types of infections in the central nervous system with an incidence of about 1 in 100,000 persons per year. This is the type of imaging we see just like in this case. A nidus of infection with surrounding edema, a vigorous inflammatory response, it enhances with contrast and very importantly the diffusion weighted image shows prominent diffusion restriction, a highly proteinaceous material and fluid in the middle of this abscess that lights up with diffusion signal. And that's the imaging signature of an abscess. Etiology is really important when evaluating patients with cerebritis or a brain abscess. Meningitis, we don't always figure out where that comes from. 01:34 Encephalitis, we often don't find where that arose. But for cerebritis and an abscess, we've got to figure out how this process, how this infection got on to the brain. And there are 3 things we think about. The first is direct or adjacent spread and this may occur because of a mastoiditis and otitis or a sinusitis. Hematogenous spread. Spread from the heart, from a valve in the heart, an infected valve in the heart, hematogenous spread is the second most common reason for a brain abscess or cerebritis to develop. We can see this after procedures, particularly neurosurgical interventions, and occasionally we don't find the source and we say that it's a cryptogenic origin or cryptogenic cerebritis. Let's think more about each of these. 02:19 For otitis and mastoiditis, that makes up about the most common cause for a cerebritis, 33% of cases of an intracranial abscess will occur because of direct spread from an ear infection or a mastoid infection. There's a predilection for the temporal lobe, typically these infections occur in the temporal lobe which is adjacent to where the ear, the inner ear, and the mastoid sinuses are. Common organisms include streptococcus, bacteroides, and pseudomonas. We think about those and we cover for those in our treatment. What about the paranasal sinuses? We can see it directly spread from the paranasal sinuses and those abscesses typically occur in the frontal lobe. We think about the same organisms that cause otitis, Staph aureus and haemophilus. And then hematogenous spread. This makes up about 25% of cases and is an important cause and guidance in treating these patients. How do patients present? What are the typical clinical symptoms of cerebritis or a brain abscess? Well, it's highly variable and it depends on the location of the focal infection in the brain. The classic triad is headache, fever, and a focal neurologic deficit but this is only present in about 50% of cases. Headache is common, present in 75% of patients, but a lot of reasons. Patients have headaches for a lot of reasons and so that's not very specific for this diagnosis. Focal deficits occur in 60% of patients and this is highly important and should guide us to getting imaging in these patients. We can see aphasia, hemiparesis, visual field cut, any focal neurologic deficit depending on the location of the infection. And seizures are not uncommon, 15% to up to 35% of patients will present with some type of seizure particularly when that infection involves the outer cortical surface. Importantly, most patients don't present quickly and on average patients wait 11-12 days while symptoms smolder, trying to figure out what's going on until their ultimate presentation. So what do we do? How do we evaluate a focal infection in the brain? Well patients that present with a focal neurologic deficit require imaging and so typically these patients have imaging prior to any type of spinal fluid tap or other assessment and usually that's sufficient to establish the diagnosis. The T1 weighted gadolinium-enhanced imaging is most important for evaluating a focal infection in the brain and here we see the typical signature for a brain abscess. On the far left, you have the axial then coronal and sagittal imaging and we see a ring-enhancing lesion. Enhancement means acute, it means this process just begun and could be an acute infection, inflammatory or malignant process. 05:04 Typically, the enhancing pattern we see with an inflammation with MS or an acute inflammatory lesion is an incomplete ring of enhancement and here you see a complete ring of enhancement. 05:15 Infection and malignancy look very similar and this is where the diffusion weighted image is helpful. Most cancers do not cause prominent diffusion restriction and we do see restricted diffusion in the inner area of an abscess. And that's the imaging signature or sequence for an abscess. How do we treat cerebritis or brain abscess? The treatment is a little bit different than what we've discussed with meningitis or cerebritis. Empiric treatment includes vancomycin for gram positive coverage and Rocephin and Flagyl for broad gram negative and atypical coverage. After a neurosurgical procedure, typically vancomycin and the 3rd generation cephalosporin like Rocephin or ceftriaxone is considered. With hematogenous spread, we consider other potential organisms. Ampicillin and sulbactam is commonly used with or without Rocephin and Flagyl. The important thing to remember is the treatment has to be prolonged. 06:11 It's hard to get antibiotic coverage into this walled-off infection. So typically the duration is 4-6 weeks. Surgery is indicated for certain types of brain abscesses particularly those that are large where there is gas, abscesses that have loculation or that are loculated, abscesses in the posterior fossa which can obstruct CSF flow and when a fungal organism is suspected or confirmed.
About the Lecture
The lecture Cerebritis and Brain Abscess by Roy Strowd, MD is from the course CNS Infections.
Included Quiz Questions
Frontal lobe abscesses commonly originate from an infection in...?
- ...the paranasal sinus.
- ...the mastoid process.
- ...the heart valves.
- ...the ear.
- ...the lungs.
Which of the following differentiates brain abscess from a neoplastic tumor on MRI?
- Diffusion restriction is more common in abscess.
- Contrast enhancement
- Lesion size
- Number of lesions
- Lesion location
Which of the following is an indication for surgical treatment of brain abscesses?
- Abscess size > 2.5 cm
- Multiple abscesses
- Abscess located in the frontal lobe
- Postsurgical abscess
- Good initial clinical condition
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |