Playlist
Show Playlist
Hide Playlist
Biochemistry of Megaloblastic Anemia
-
Slides Macrocytic Deficiency.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
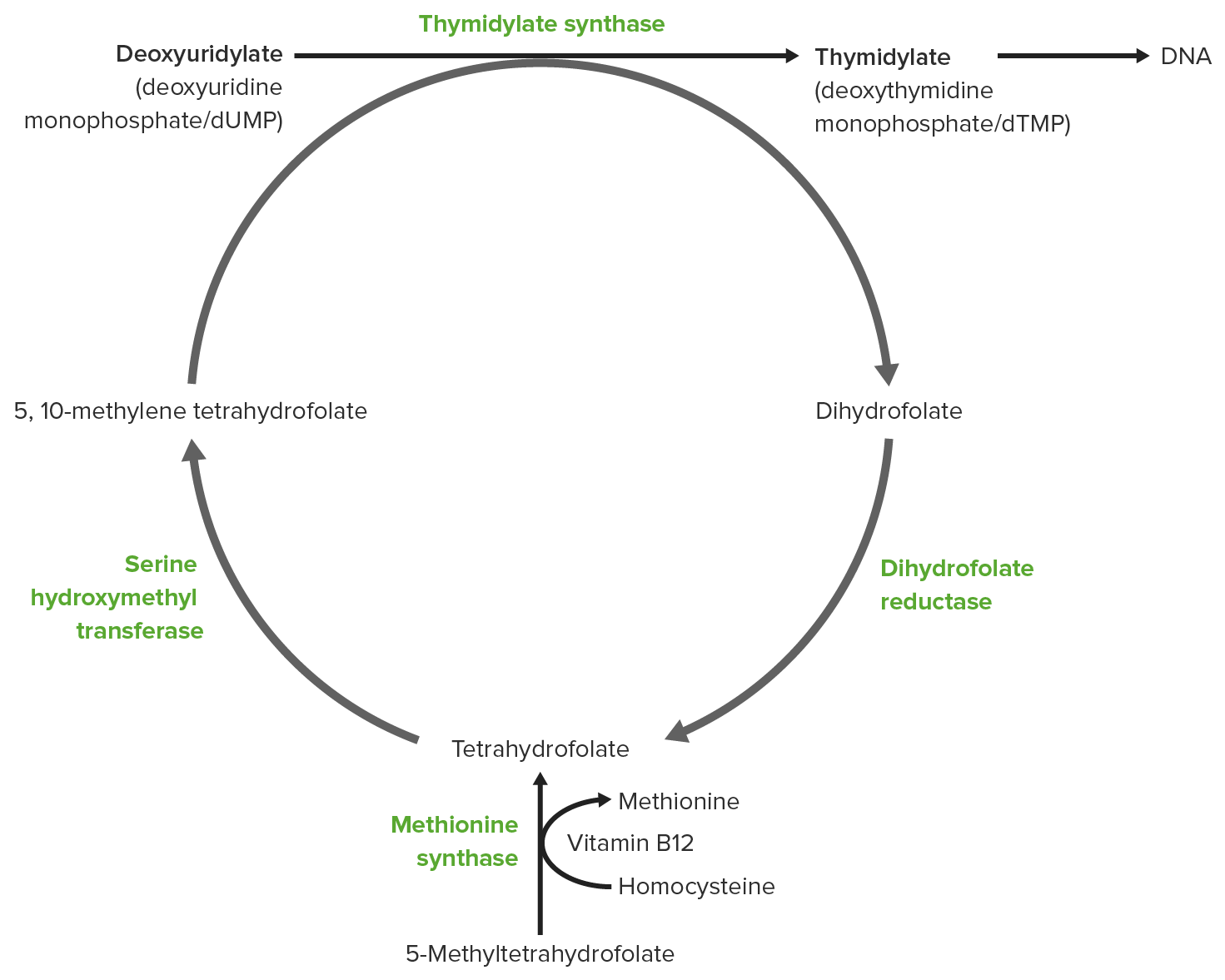
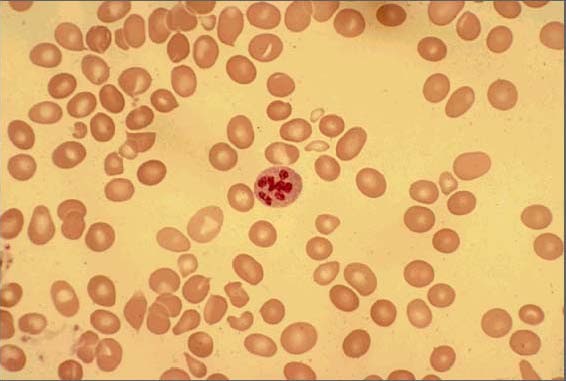
00:00 Let's take a look at causes of megaloblastic anemia. 00:03 Now, once we've complete the discussion of megaloblastic, I'm gonna mention some of these non-megaloblast. 00:09 Megaloblastic anemia, now I'm gonna set this up for you. 00:12 It is an important slide, a lot of things that are occurring here. 00:15 First, let's take a look at the peripheral blood smear and what you end up seeing there are megaloblast. 00:21 Look how large they are, highly nucleated and lack of proper maturation. 00:26 Those are RBCs, can you believe that? Those RBCs? Yeah, or in other words it's primitive cells and you should never have an RBC that looks like that, right? I mean the nucleus shouldn't be there, it should be central pallor, so on and so forth, but that isn't occurring. 00:41 Now, let me set this up. I'm gonna slow down here a little bit and make sure that you're very, very familiar with these two pictures and I'm gonna tell you as to how to use these, okay? The top picture, for the most part, we're gonna go from the diet and we're gonna consume let's say folate and we're gonna then interact with B12 and when we interact with B12 then I'm gonna walk you through what's known as tetrahydrofolate and then have you really take a look at that first picture here, and the objective is to convert your dUMP into dTMP, right? What does that mean to you? Well, you know from genetics, once again, that if you wanna form DNA you can't have UMP, you can't have uracil, you need to convert that U into what? Good. Your tri or your thymidine. 01:28 And so therefore, this is the objective and what we're gonna do here is we're gonna interplay both B12 and folate, so we can form a dTMP. Is that clear? Okay. 01:40 So, that's the first picture and then on the second picture, I will elucidate that further. 01:46 Okay, let's begin at the top. 01:48 You are now consuming folate, what you're taking in is going to be that form that you see there, at least pay attention to the methyl, please; the f stands for folate, h stands for tetra, so there you go, tetrahydrofolate attached with the methyl, we don't need methyl in order for proper action and functioning, so we need to find a way to remove that methyl and give to a acceptor and so it will donate the methyl, something's gonna accept it and you'll see this now. 02:18 So what is this acceptor of the methyl, because if you don't accept the methyl, then you basically have inactive folate, do you understand that? And where are you getting this from? The diet. 02:28 Okay, so that'll be greens and so and so forth. 02:31 So you've taken in the methyltetrahydrofolate, you're going to then donate the methyl to the B12, look at the B12 there, it says methyl B12. 02:40 So we have to have B12 communicating or interacting with the folate so that it can accept the methyl. 02:47 Now, what are you gonna do? Now, the B12 is going to donate that methyl to the homocysteine and the enzyme there is called methionine synthase. 02:57 Wow, how appropriate is that? Quite. 03:00 So the methyl will be donated to methionine synthase or with the help of methionine synthase will then convert homocysteine into methionine. Stop there. 03:08 Clinically, you as a clinician, what are you gonna look for in the urine to help you suspect or even perhaps confirm megaloblastic anemia being caused by B12 or folate? Now, what I must bring to attention is that you're going to find hyperhomocysteinemia and hyperhomocysteinuria in both folate and B12. 03:31 Say that three times fast, it's quite fun. 03:33 Ready. Hyperhomocysteinuria, hyperhomocysteinemia. 03:37 So now you have tons of homocysteine in the urine, but all that it's told you now is that I have megaloblastic anemia being caused only by B12? Only by folate? Or both? Both. 03:52 So all these tells you is that you have megaloblastic anemia being caused by either B12 or folate, but you don't know which one, why? Look, if you're not taking your methyl, alright, so from the diet, if you're not taking your methyltetrahydrofolate, how could you possibly convert your homocysteine into methionine? You cannot. So in folate deficiency, please, listen, fact, you do have hyperhomocysteinemia and you will have hyperhomocysteinuria. 04:19 Number two, what if you didn't have B12? If you didn't have B12, first it wouldn't accept the methyl; secondly, methionine synthase really wouldn't be working. 04:31 You should know that B12 is a cofactor for methionine synthase. Interesting. 04:36 So if that enzyme isn't working and it's not accepting the methyl, B12 deficiency results in? Good. Hyperhomocysteinemia, hyperhomocysteinuria. 04:46 All that tells you is megaloblastic anemia. 04:48 Now, hyperhomocysteinemia from biochemistry you should know about other things including your ornithine and stuff like that but cystathionine synthase and I'm not gonna bring all that here though. Biochem, look up cystathionine, that's important. 05:02 Next, alright now, everything goes well. 05:06 The methyl comes in taken up by B12 and it's properly handled. Your left with tetrahydrofolate. Now what do you do? Well, that tetrahydrofolate, if I we're you I would know some of these cofactors and these include your serine and glycine, and you're gonna then form what's known as methylenetetrahydrofolate, now this is the usable form. Pay attention here. 05:27 You have an interesting enzyme here. It's called thymidylate synthase. 05:31 Thymidylate synthase is then going to take that tetrahydrofolate, accept two of them, to what? Well, you have four, right? Tetrahydrofolate, it will take up two and so take up the two folate and convert the dUMP to dTMP, you must know the enzyme, thymidylate synthase I'll tell you one a second, many of you already know. 05:52 So now you're left with? You're left with dihydrofolate. 05:55 Aah, I know you've heard of that. Dihydrofolate. 05:58 And what are you gonna do in biochemistry with dihydrofolate? You're gonna reduce it, aren't you? When you reduce, whenever reduction type of formula or calculation in biochemistry, it actually means you're gonna increase it. Ridiculous, but anyhow. 06:12 So you're gonna reduce this dihydrofolate with the help of what enzyme? You all know about dihydrofolate reductase. 06:19 There it is, look, you reduced it with reductase. 06:21 So now you took the dihydrofolate and you convert it into tetrahydrofolate. 06:25 That rises all this necessary more than you can imagine. Watch. 06:29 So my topic is B12 folate deficiency, we're gonna put in the drugs here, we're gonna put in some pathology here and then once we are done with this picture, we're gonna move to another one and I'm not gonna bring it up now though, but it's important. 06:41 Let's begin. Say that your patient has cancer, unfortunately, and you're thinking about giving them a antineoplastic drug called methotrexate, take a look at MTX identified here. 06:53 MTX is methotrexate; high dose of methotrexate has been given. 06:58 It's mechanism of action is to inhibit dihydrofolate reductase, in what kind of cells? Yeah, cancer cells, right? And if you inhibit this enzyme you can't properly what? Recycle your folate so therefore you can't form dTMP. 07:14 What happens to this cancer cell, it dies. Chemotherapy. 07:19 Is it possible that methotrexate might bleed over into a normal cell? Of course, you already know this as well. You do? Mm-hmm. 07:26 What's the name of that rescue? Leucovorin rescue. 07:31 What's the name of that folate? It's called folinic acid. All this come together? I hope so. 07:37 So here's methotrexate, it inhibits the enzyme dihydrofolate reductase, okay? Good, now what? I can't properly reduce my dihydrofolate, for all intent and purpose is you are folate deficient. 07:49 If this bleeds into a normal human cell, eukaryotic, then you know, that you're folate deficient. 07:56 What does this result in, please? Megaloblastic anemia. 07:59 If it's high dose, what are gonna give this patient to then replenish their folate in the human cells only, without affecting the cancer cells? It's called folinic acid. 08:09 Give me the technical name or give me the, I guess, the trade name, that's leucovorin or leucovorin rescue. 08:16 Drug number one. What's TMP? Trimethoprim. 08:20 Who are you trying to combat here? Bacteria, right? It's an antibiotic. 08:25 Same concept, here's an antibiotic that you're giving. Have you heard of cotrimoxazole, haven't you? That's sulfamethoxazole plus your? Good, trimethoprim. so you have cotrimoxazole. 08:35 So this is a drug that you're going to give to kill off bacteria. 08:39 It inhibits dihydrofolate reductase in that bacteria, kills off the bacteria, unfortunately, might also cause humans cells to die, for the same reason, is that clear? So both of these results in what kind of deficiency? Folate deficiency. 08:52 What kind of anemia is the patient going to suffer from? Good, that's your megaloblastic anemia. What do you want to do with this patient? Either, well, as we said, leucovorin or remove the drug if need be, right? Change the drug, so on and so forth. 09:05 Two down with drugs. Let's talk about the third one. 09:08 Here's my thymidylate synthase, recognize it, you see it? Okay. 09:12 That converts your dUMP into dTMP and it takes up two of your folates so they form dihydrofolate. 09:22 So 5-FU is 5-Fluorouracil, that the drug also antineoplastic, it inhibits the enzyme thymidylate synthase, here once again, for all intent and purposes, please know, that you're going to then become folate deficient, it's important. 09:38 The only thing that I wish to bring to your attention, current day practice, that if you use FU, you don't have to give leucovorin. 09:46 In fact, if you give FU, it's just the opposite, it is going to then enhance the activity -- enhance the activity, keep that in mind. 09:54 And so, therefore, there's no such thing as giving this patient leucovorin to save the overdose of 5-FU, keep that in mind, especially when you're dealing with drugs later on in pharmacology, trying to treat a patient with colorectal cancer, that's a big one. Don't forget that, please. 10:11 We'll have discussions more and we've talked about this in neoplasia as well. 10:17 So those are the big drugs. Know those inhibitions, know those enzymes, there's interplay between folate and B12 and that's the first picture. 10:25 In the second picture, this entire biochemical pathway has nothing to do with these drugs, it has nothing to do with really dietary issue, and what it really deals with only is true B12 deficiency. 10:39 You tell me about a patient clinically that's presenting a B12 deficiency and which folate deficient patient will never present with? What happens here? Walking wide stance, I close my eyes I don't know where I am, and I have upper motor neuron lesion, right? What the heck is all these? It's called subacute combined degeneration. 11:06 Let's go step by step. 11:07 Wide stance, I'm walking towards you but wide ataxia, ataxic gate. 11:13 So what organ in your brain controls your coordination? Good. Cerebellum, and so therefore your spine or cerebellar tract is knocked out. 11:23 Number one, I mean another one, I said I close my eyes and I'm moving, I'm swaying, I'm vibrating, not vibrating, I can't vibrate, and this is what? Proprioception. 11:35 So I don't have -- loss of touch, loss of proprioception, I'm doing positive Romberg, right? I close my eyes but I've lost all spatial orientation and I get, you know, I just can't stand still -- stability has been lost, which column is that? Good. Dorsal column, two down. 11:52 And what's this? Like rigidity almost, that's upper motor lesion. 11:57 Spastic paralysis. That is going to be? Good, lateral corticospinal tract. 12:02 All three tracts you must know, what's it called? Subacute slowly combined three tracts -- lateral corticospinal, spinal cerebellar, and dorsal column degeneration. 12:15 What's degenerating in those columns or in those tracts? The myelin, right? Good, you only find that in B12 deficiency, you never find that in folate. Clear? What about this, demyelin disorder? Irreversible, keep that in mind. 12:30 If you don't give a simple injection of B12 in your butt, meaning intramuscular, then understand you go through irreversible deterioration of your patient. That's your patient. 12:43 Let's take a look at the biochemistry. Identify the B12. Interesting. 12:48 So here the B12 is also a cofactor for a second enzyme beginning with the letter M, this are called methylmalonyl CoA mutase. 12:57 What is the other one, Dr. Raj? Well, you tell me. That was called methionine synthase. 13:03 When methionine synthase was knocked out, your patient with B12 results in hyperhomocysteinemia. 13:10 This is methylmalonyl CoA mutase. 13:13 So what are you gonna find here in this patient that you will never find in folate deficient? Good. Methylmalonic aciduria, right? How would you ever find this in a folate deficiency? There's nothing please, take a look at this. 13:28 There's nothing in this formula here that has folate in it, okay? Now, so what's causing the demyelination? Whenever you knock out an enzyme, would you tell me what happens to the proximal substrate always? Yeah, it increases. Keep going back. 13:42 So we talked about MMA which methylmalonyl CoA aciduria, and then keep going back, are you gonna increase propionyl CoA? Of course, you are. Okay, now what do you need to properly myelinate your nerve? Take a look at that, what's in bold there? You need acetyl CoA, for normal myelin synthesis. 14:01 Now, I have too much propionyl CoA. Guess what? It replaces the acetyl CoA and you demyelinate. What are the tracts? Spinal cerebellar, ataxic gait; upper motor neuron lesion, that's your lateral corticospinal tract; and positive Romberg, and no vibration or touch, that is your dorsal column. Clear? Now the only thing that I'll make sure that we're clear here from biochemistry is that you are going to take up the propionyl CoA pathway if everything is perfectly normal and you had enough of your what's known as your biotin and you had enough of your B12 and you kept going, then you're going to your TCA, tricyclic or Krebs cycle, right? But what kind of fat would you be taking up? It's called odd chain fatty acids, keep that in mind because the board love those questions about odd chain, you've heard of long chain and short chain and medium chain, especially medium chain, they love that one. 14:57 But keep in mind though that odd chain fatty acids that you're going to take up. That's important. 15:02 Now, I only have a little thing that I wish to bring to your attention here, it's a nice little figure, it really is because it integrates a lot of stuff is that anytime that you find carboxylase in biochemistry, any pathway, the cofactor here is biotin, is that clear? Biotin. 15:19 So they say that if Im able to consume, on a personal note, if I'm able to consume enough biotin and I reeved up my biotin levels in my body, I'm supposed to have hair growth, yet to see that, right? So anyhow, biotin is rather interesting. Know that it's being one of those cofactors for carboxylase. 15:36 Here however, if you have B12 deficiency, you undergo demyelination and you find methylmalonic aciduria in folate. 15:45 We've spend a lot of time on these figures, a lot of questions come from these. 15:49 And a lot of integration as you can see, your biochemistry, pharmacology, pathology. 15:53 Ultimately, what are we dealing with? Macrocytic greater than 100 MCV. 15:58 Megaloblastic or non-megaloblastic? Good. Megaloblastic.
About the Lecture
The lecture Biochemistry of Megaloblastic Anemia by Carlo Raj, MD is from the course Macrocytic Anemia – Red Blood Cell Pathology (RBC).
Included Quiz Questions
Which of the following prevents megaloblastic anemia in patients taking methotrexate?
- Folinic acid
- Ascorbic acid
- Iron
- Vitamin B12
- Retinoic acid
Orotic aciduria due to uridine monophosphate synthetase deficiency follows which of the following inheritance patterns?
- Autosomal recessive
- Autosomal dominant
- Chromosomal inheritance
- X-linked dominant
- X-linked recessive
Why does demyelination occur in vitamin B12 deficiency?
- Propionyl CoA replaces acetyl CoA in neuronal membranes.
- Acetyl CoA replaces Propionyl CoA in neuronal membranes.
- Increased blood levels of succinyl-CoA.
- Decreased blood levels of methylmalonic acid.
- Increased blood levels of homocysteine.
Customer reviews
4,2 of 5 stars
| 5 Stars |
|
4 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
1 |
Dr. Raj has the ability to break down incredibly complex pathophysiologic mechanisms into easy-to-digest pieces!
I´LOVE DE WAY HE EXPLAINS MEDICINE. he is fun, makes everything simple
The name of the lecture was very contradicting to the material given. In addition, I felt that the explanation as everywhere there was no proper structure of things.
Î really appreciate the Lectures, this whole Website helps a lot. But it´s annoying that the Professor always says " repeat it 3 times fast " , Theres no point in doing that , if nobody could understand him in the first place . If you cant properly spell it out /pronounce it one time, it´s no use to repeat it fast.
1 customer review without text
1 user review without text