Playlist
Show Playlist
Hide Playlist
Brain Abscess: Pathology
-
Slides BrainAbscess InfectiousDiseases.pdf
-
Reference List Infectious Diseases.pdf
-
Download Lecture Overview
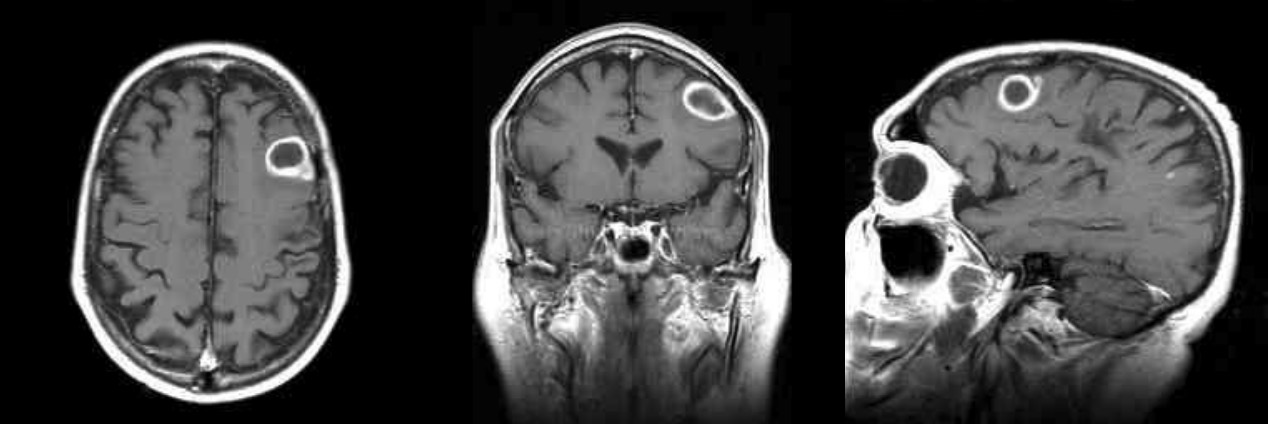
00:01 So, how do the organisms reach the brain? Well, they reach the brain in a variety of ways as a result of a contiguous focus of infection. 00:10 For example, otitis media or mastoiditis. 00:14 And you would expect the abscess to be nearby in the temporal lobe or the cerebellum. 00:22 Sinusitis can be a cause of a brain abscess, either frontal or sphenoid sinus, and you would expect the frontal lobe to be most likely involved. 00:33 And we already talked about penetrating trauma anywhere in the brain. 00:39 Now, after neurosurgery, brain abscess does occasionally occur. 00:46 But more commonly, it would be the result of hematogenous dissemination from a lung abscess and empyema or bronchiectasis. 00:56 There is an association with those pus-containing lung cavities. 01:02 We've already mentioned infective endocarditis. 01:06 Neutropenia, patients who have very low levels of white blood cells are particularly prone to bloodstream infections. 01:16 And abscess in the brain is not that common and the reason they don't get abscess is because they don't have much in the way of white cells to make an abscess. 01:29 So, more often in a neutropenic patient, it would be cerebritis. 01:35 Cyanotic congenital heart disease, these patients can certainly get brain abscesses more commonly than normal folks do. 01:47 And the same thing goes for hereditary hemorrhagic telangiectasia. 01:53 Protozoa, free-living amoeba, we’ve talked about in helminths. 01:59 So, what are then the stages of brain abscess evolution if we turn to the pathogenesis. 02:05 Well, first of all, in the first three days, you're going to have simply cerebritis. 02:10 You're not going to have a well-formed abscess. 02:15 Later on, you have the beginnings of an abscess, but it takes 10 to 13 days to develop a reasonable capsule around it and 14 or more days to get a thickened capsule. 02:34 And in terms of where a neurosurgeon would try to drain it, they would normally wait until there's a well-formed capsule after a couple of weeks. 02:46 So, you wouldn't want to go in to the stage of early cerebritis if you were a neurosurgeon because it would be hard to define where the infection actually was.
About the Lecture
The lecture Brain Abscess: Pathology by John Fisher, MD is from the course CNS Infection—Infectious Diseases.
Included Quiz Questions
Where in the brain would you typically expect to see an abscess if it is formed by contiguous spread of otitis media?
- Temporal lobe
- Frontal lobe
- Parietal lobe
- Occipital lobe
- Central fissure
At approximately what point during the pathogenesis of a brain abscess does the lesion become surrounded by a fibrotic capsule?
- After 2 weeks
- Within the first 3 days
- Within the first week
- After 2 months
- Within the first hour
Which of the following best describes the usual way of managing a brain abscess?
- A combination of antibiotics and surgical drainage for both diagnostic and therapeutic purposes
- A combination of antibiotics and surgical drainage only for therapeutic purposes
- Antibiotics without surgical drainage
- Surgical drainage without antibiotics
- Surgical drainage only for diagnosis followed by antibiotic therapy
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |