Playlist
Show Playlist
Hide Playlist
Brain Abscess: Initial Management
-
Slides BrainAbscess InfectiousDiseases.pdf
-
Reference List Infectious Diseases.pdf
-
Download Lecture Overview
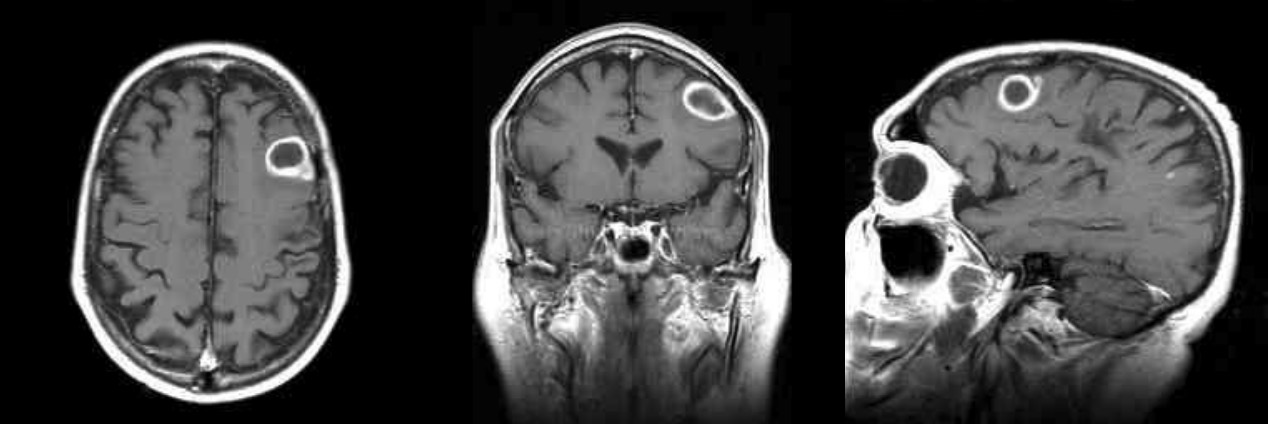
00:01 So, the initial management for lesions that are greater than 2 cm are going to be surgical excision. 00:09 But remember, we need a well- formed abscess to surgically excise it and they do that with stereotactic aspiration. 00:18 And then, empirical therapy is going to be based on the predisposing condition. 00:24 The microscopy of abscess contents, results of blood cultures, and certainly many of these patients would be given phenytoin to prevent seizures. 00:37 So, the initial management of a brain abscess was going to be six to eight weeks of IV therapy, followed by most likely two to three months of oral treatment, but it does depend. 00:49 If it's mixed infection, we’re going to start with high-dose IV penicillin. 00:54 You need the highest dose to cross the blood-brain barrier and penetrate the abscess or maybe a third-generation cephalosporin. 01:02 And we’re going to add metronidazole to that. 01:05 It gets spectacular levels in brain parenchyma and it is probably the best agent we have as a single agent for anaerobes. 01:17 If we know it’s Staph aureus on the basis of the Gram stain, we’re going to give IV vancomycin until we find out whether it's MRSA or not. 01:28 If it's not MRSA, we can back off to a more narrow spectrum nafcillin or oxycillin. 01:35 Now, if the patient has a penicillin allergy, we’re looking at a cephalosporin like ceftriaxone which penetrates into the spinal fluid better than other cephalosporins. 01:47 If it Pseudomonas aeruginosa we’re talking about ceftazidime or cefepime and the Gram stain would show you myriads of gram-negative rods. 01:59 And so, the gold standard is going to be six to eight weeks again of IV therapy, followed by months. 02:08 Now, if it’s Nocardia, we’re going to start with trim sulfa. 02:14 And the total duration of therapy is going to be actually 12 months for Nocardia. 02:21 If the patient has a treatment failure, we may have to add a carbapenem, a third-generation cephalosporin, minocycline or Linezolid. 02:31 If it's of unclear etiology, we need vancomycin to cover the staphylococci. 02:37 We need metronidazole to cover the anaerobes. 02:40 And we need ceftriaxone to cover the aerobic gram-negative rods. 02:45 If we’re worried about Pseudomonas, then we would change from ceftriaxone to cefepime for that particular organism. 02:55 If it's a fungal brain abscess and we have evidence of, for example, Candida, we start out with liposomal amphotericin B plus flucytosine. 03:06 And then when the patient is stable or improving, we switch over to fluconazole. 03:13 If it's Aspergillus or Scedosporium, the drug of choice is going to be voriconazole. 03:19 And that is given until there is absolutely no evidence of a brain abscess. 03:27 For the zygomycetes, we’re going to use – and these are the bread molds, the Rhizopus, we’re going to be using amphotericin B. 03:36 And then, after the patient has improved, transitioning to an azole known as posaconazole. 03:44 Some people suggest we should use hyperbaric oxygen, but the studies demonstrating the effectiveness of this therapy are rather small, and so that remains controversial. 03:58 For Toxoplasma gondii, it's pyrimethamine plus sulfadiazine for at least six weeks, followed by suppressive therapy. 04:08 If the patient is allergic to sulfur drugs, we use clindamycin. 04:12 For Taenia solium causing cysticercosis, this is controversial. 04:23 What you're looking at are the cysts, the tissue cysts from cysticercosis. 04:31 And by the way, if a Mexican immigrant comes into the United States and has a first time seizure as an adult, this is the most common cause of that. 04:46 So, cysticercosis should be suspected. 04:48 But at any rate, if this diagnosis is made, you have to remember that some of these cysts contain living organisms. 04:57 So, if you give them something that would kill the organism, you are going to create a tremendous amount of inflammation and brain swelling. 05:07 So, the brain inside that solid skull doesn't have any room to swell, so you may actually cause increased intracranial pressure and herniation. 05:17 So, it's very, very controversial as to whether to treat it at least initially. 05:25 Most people recommend that you start albendazole or or praziquantel and then you give dexamethasone. 05:36 And that brings me to my conclusion of speaking about brain abscess.
About the Lecture
The lecture Brain Abscess: Initial Management by John Fisher, MD is from the course CNS Infection—Infectious Diseases. It contains the following chapters:
- Initial Management
- Antimicrobial Therapy
Included Quiz Questions
Which of the following types of surgery is generally preferred for the treatment of brain abscess?
- Needle aspiration
- Surgical excision
- Intralesional injection of alcohol
- Intralesional injection of antibiotics
- Surgical therapy has no role in the treatment of brain abscess.
For a staphylococcal brain abscess, what is the typical duration of intravenous antibiotic therapy?
- 6-8 weeks
- 2-3 weeks
- 2-3 months
- 6 months
- 5-10 days
What is the initial treatment for a brain abscess due to Nocardia?
- Trimethoprim/sulfamethoxazole up to 12 months
- Trimethoprim/sulfamethoxazole for 6 weeks
- Carbapenem for 12 months
- Linezolid for 2 months
- Carbapenem for 2 weeks
Which of the following is the most appropriate empiric therapy for brain abscess following traumatic brain injury involving the paranasal sinuses?
- Vancomycin, metronidazole, and cefepime
- Metronidazole, cefepime, ciprofloxacin
- Cefepime, ciprofloxacin, gentamicin
- Ciprofloxacin, gentamicin, vancomycin
- Gentamycin, vancomycin, metronidazole
What is the anti-fungal treatment of choice when treating an Aspirgillus brain abscess?
- Voriconazole
- Fluconazole
- Liposomal amphotericin B
- Posaconazole
- Flucytosine
What is the most common parasitic nervous system infection in the developing world and the leading cause of acquired epilepsy?
- Neurocysticercosis
- Toxoplasmosis
- Schistosomiasis
- Echinococcosis
- Coenurosis
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Thank You sir i really enjoyed your lecture. i hope to see more lectures by you.