Playlist
Show Playlist
Hide Playlist
Beta Thalassemia: Morphology and Hemoglobin Electrophoresis
-
Slides Anemia Alpha Beta Thalassemia.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
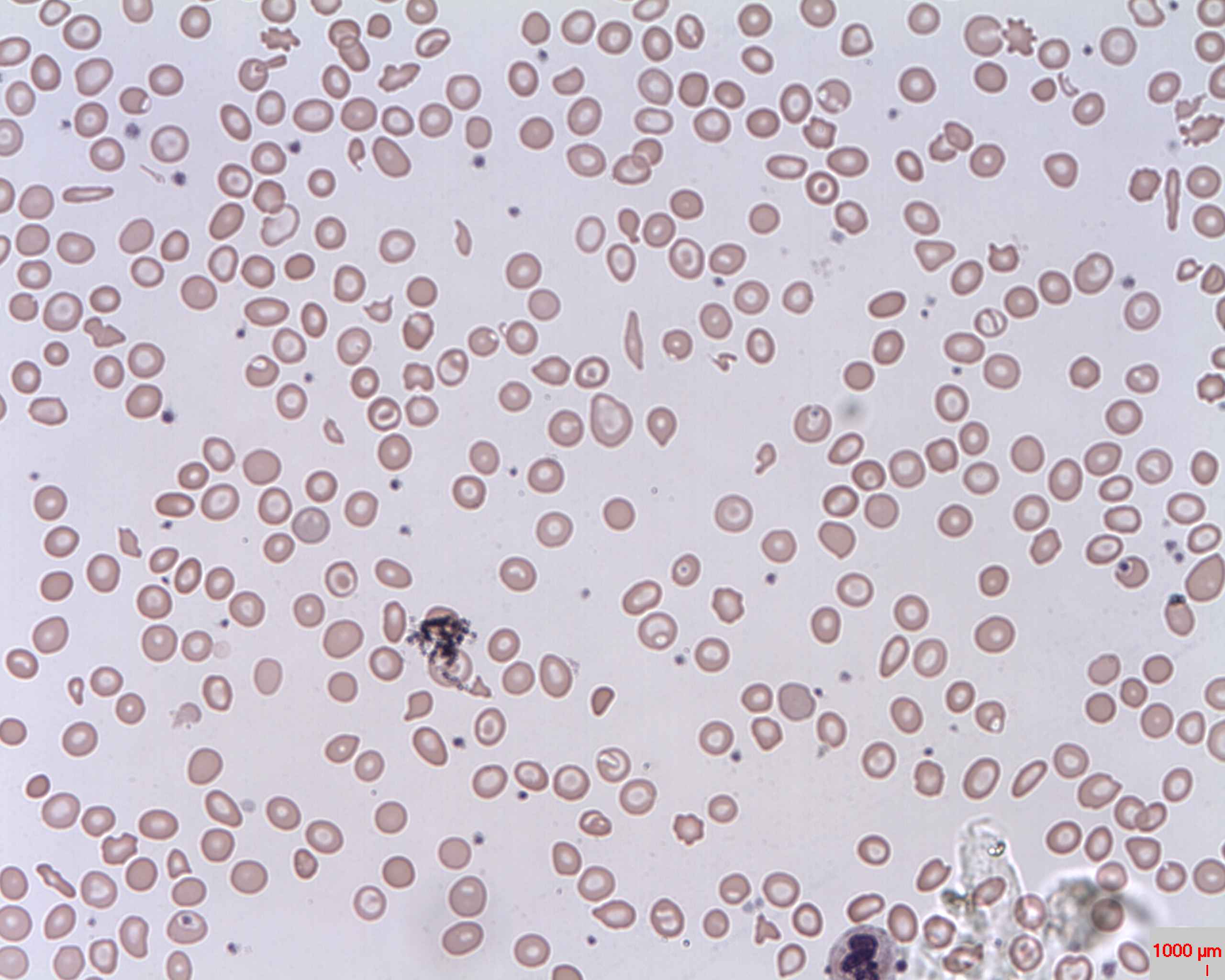
00:00 The morphology here is going to be rather all over the place, so maybe you find microcytic hypochromic, maybe you find teardrop cells, maybe you find nucleated RBCs. 00:09 It's a rather broad type of picture and you can kinda see some of these in here as well, you can maybe find target cells. 00:15 So a very, very -- what's known as anisopoikilocytosis or anisocytosis. 00:21 You're gonna have all kinds of variations in terms of your peripheral blood smear. 00:26 Be careful. Okay, this is both for beta and alpha hence, I've just put it here so you can use this picture for both alpha and beta. 00:34 Anisopoikilocytosis and target cells, you know, all kinds of RBCS. 00:39 Okay, now let's take a look at that hemoglobin electrophoresis that I've been referring to as and we have two types that we're gonna pay attention to, that's it, either a minor or major. 00:50 Let's take a look at minor first, please. That would be the top row. 00:54 So, beta-thal minor, here what happens, while you don't produce as much beta-globin now, you tell me. Close your eyes. 01:01 What's a normal hemoglobin A? Good, 97%. 01:06 And so, therefore, it's minor. Are you able to produce as much hemoglobin A? No, take a look at the percentage. There you go, 93%. 01:14 That's why I wanted you to memorize normal. 01:16 Do not waste your time memorizing these. 01:18 Take a look at normal and then you should be able to figure out what's going on with your patient. 01:23 Now, close your eyes again. What's your normal hemoglobin A2? You know I'm doing that. And hemoglobin F. 01:31 Normally, hemoglobin A2 was 2%, hemoglobin F was 1%. 01:36 Take a look at your percentages here, two went up to five, one went up to two. 01:43 Compensation. Why? Because hemoglobin A2 and F does not have or do not require betaglobins. 01:51 Let's go to major. In major, what happens? Good, no hemoglobin A. 01:57 Take a look at hemoglobin A, blank slate. And then who compensates? It'll be hemoglobin F that compensates quite a bit. Quite a bit. 02:06 Now, can we live with -- as we as -- you and I as adults, remember this hemoglobin F, this is not a baby, this is not a fetus, okay? This is you and I, an adult, hopefully. 02:17 So, as an adult, you have hemoglobin F, wow. Where is all your oxygen? It's a left shift of your oxygen dissociation curve, therefore, my oxygen is stuck on my hemoglobin. 02:31 So, what about my tissue? Starving. Absolutely starving, right? So what must you do with this patient? Good, transfusion. You have to. 02:41 You have no other choice. 02:42 Now, if you're gonna give transfusion over and over and over again, what does that mean? Packed RBCs. RBCs contain quite a bit of iron, so what are you always monitoring in the patient in which you give transfusion? Iron, iron, iron, iron. What if you don't give transfusion? This child is gonna die. Okay? The child is gonna die. But if you repeat the -- and then now, you have to begin transfusion, don't you? So, as you begin transfusion, let's say it's going on for 15 or 20 years. 03:12 So, even if you try to control that iron, unfortunately, it's difficult. 03:18 And so, now, what happens? Excess iron and then it starts doing what? Starts accumulating on your heart. 03:25 Oh, boy. And now, let's say at the age of 23, the patient with beta-thal major dies. 03:31 What did the patient die of? Heart disease. 03:34 You might notice being restrictive, which is perfectly fine, but please don't forget, it could very well be dilated. 03:41 So, it could be either a restrictive cardiomyopathy or dilated cardiomyopathy. 03:46 A heart disease that a patient will die of, called what? Secondary hemochromatosis causing heart disease, but in addition, iron is also going to accumulate on the skin, it might also on the pancreas, diabetes, look for hyperglycemia. 04:02 Do you see as to how much more information there is with beta-thalassemia major? And it's important that you understand everything else that we talked about here, along with the complications with transfusions.
About the Lecture
The lecture Beta Thalassemia: Morphology and Hemoglobin Electrophoresis by Carlo Raj, MD is from the course Microcytic Anemia – Red Blood Cell Pathology (RBC).
Included Quiz Questions
Mainly which type of hemoglobin is increased in beta thalassemia minor?
- Hemoglobin A2
- Hemoglobin H
- Hemoglobin Barts
- Hemoglobin F
- Hemoglobin A
Which of the following hemoglobin A2 values in a hemoglobin electrophoresis is most suggestive of beta thalassemia minor?
- 5%
- 12%
- 90%
- 65%
- 97%
Which of the following types of hemoglobin is commonly the dominant type of hemoglobin in beta thalassemia major?
- Hemoglobin F
- Hemoglobin Barts
- Hemoglobin A2
- Hemoglobin C
- Hemoglobin H
Which of the following is a common complication of transfusion-dependent beta thalassemia major?
- Secondary hemochromatosis
- Esophageal web
- Hypertrophic obstructive cardiomyopathy
- Wilson disease
- Primary hemochromatosis
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
I had troubles understanding this topic in years!!!!! Dr. Raj could explain it to me in minutes! Thank you so much! You are doing such a great work for your students!