Playlist
Show Playlist
Hide Playlist
Basics of Creatinine
-
Slides ClinicalApplicationofCreatinine RenalPathology.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
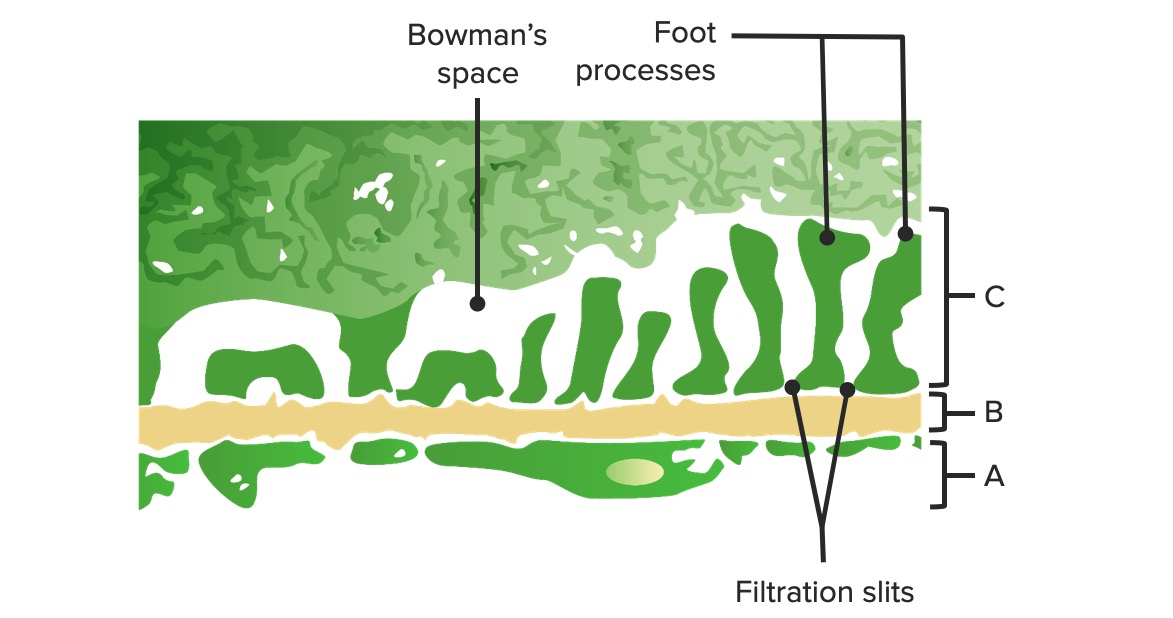
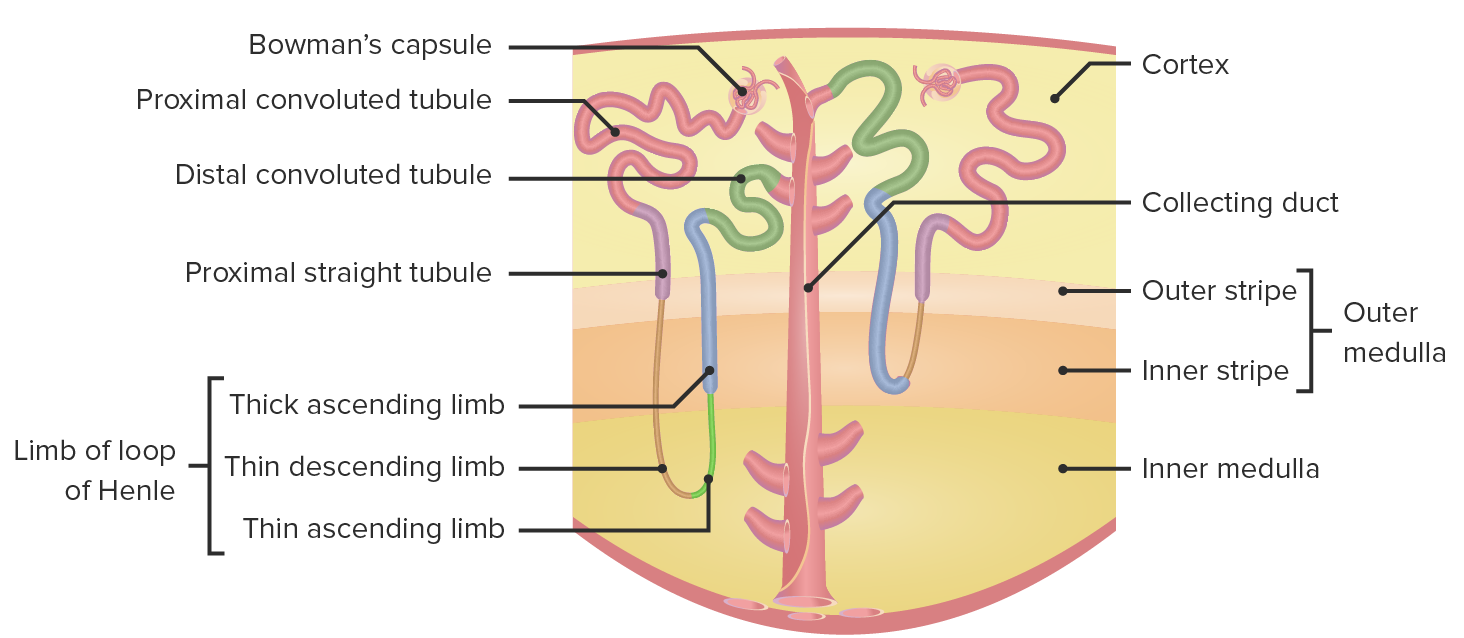
00:01 Creatinine: all the different places that you might have to run to, to look for the relevant information of creatinine. It's all here. What does that mean? What is a normal mechanics of creatinine? What does it mean to you in terms of interpretation of creatinine so that you can help you diagnose your patient? Remember this is going to be part of your laboratory investigations and is it the only thing that you are going to use to confirm. No, but it is a darn important one. What is creatinine? We will begin. The breakdown product of the skeletal muscle and how often does that occur? All the time constitutively. 00:44 Keep that in mind. Constant release into the blood stream. Once again because your muscles are breaking down you get it into your bloodstream. Remember as to what the normal levels of creatinine is? Well, I want you to think of 6 and 12. You double 6 and you get 12. It is 0.6 to approximately 1.2. Keep it simple. There is so many different things that you need to memorize, right? And a couple of things here and perhaps it may help you keep it mind, but 0.6 to 1.2. How does the kidney handle creatinine? Well, I want you to go into the plasma. I want you to go into afferent arteriole. I want you to arrive at the glomerulus and I want you to filter through. Does creatinine get filtered? Is it small enough for it to get filtered? It is. So it gets filtered. Correct. Okay? Next. 01:46 As it gets filtered, you will continue through your glomerular capillaries and you end up on the efferent arteriole, are you there? and you continue through the peritubular capillaries. We call this what? vasa recta and you tell me what should happen around the PCP, proximal convoluted tubule and its communication with the peritubular capillary. Are you with me? Are you there? Next well what kind of mechanisms are taking place between the PCT and the peritubular capillary? Two major mechanisms. One would be secretion and one would be reabsorption. Right? So of the two which process is creatinine following? Secretion. What does secretion mean? Secretion means you are always, I don't care where you are. What does that mean? You could be in the intestine. You could be here in the nephron. Secretion always means you are secreting into the lumen. What is in the lumen here? The PCP, proximal convoluted tubule and the lumen is the urine. Creatinine will be slightly secreted. Is it filtered? Yes. Is it secreted? Yes. Keep that in mind. Lets continue. 03:03 It is not reabsorbed. Is that clear? What does the reabsorption mean? Once again you could be in the GI or you could be in the nephron. Those are two major organ system where secretion, reabsorption is a major function. You want to keep these in mind. Many many pathologic conditions in which there might be excess reabsorption or excess secretion. 03:28 You will see as we walk through many differentials. Creatinine is not reabsorbed. It doesn't come back into the blood. That is important. It is only slightly secreted. So therefore when something gets filtered and it gets cleared, what does cleared mean? It is what you are actually analyzing when you get the urine out meaning to say literally and I am going to be rather dramatic here in the toilet. That is clearance. There is a difference between clearance and filtration. Filtration is you are moving from the glomerular capillaries from the afferent arteriole tuft of capillaries and into the glomerulus. That's it. That is as far as filtration goes. Is that clear? Haha, no pun intended. Clearance means what you are actually analyzing in the toilet, which you actually excreted. My point is this. So if creatinine gets filtered, does it do that? Yes. Does it get reabsorbed? No. Does it get secreted slightly? Which means that clearance would be greater than or less than or equal to GFR. That is your next big question. Think about that. Close your eyes. Listen to what I am saying. Conceptualizes right now. Clearance will be greater than GFR. What does that mean Dr. Raj? It means that because of slight secretion would be an overestimate of what is actual filtration? Now how are you as a clinician going to use all this information. Well, there is a couple of tests that you would do with creatinine, which we will then use or you will then use in practice to measure or analyze or assess the function of your kidney and there are two ways in which you can then use creatinine to assess the functionality of the kidney. 05:26 You can either use what is known as creatinine clearance, which is extremely cumbersome or you can use the surrogate marker meaning you will then measure the amount of creatinine in your plasma and how do you do that? With a blood test. Now, what is the 0.6 to 1, we were talking about that level? Is that the measurement that you are going to find as a marker in your blood or is that part of what is known as your creatinine clearance? You tell me that is your plasma, isn't it? So you can measure the 0.6 to 1.2 is a very quick general functioning assessment of the kidney that you are going to get from the blood. Keep that separate from what we see here. This is the creatinine clearance. So what does that mean? You are going to give your patient a container and you are going to tell this patient for approximately 24 hours to urinate in that container. Does that seem rather cumbersome? Sure. Does that mean that you are dependent upon the compliance of the patient? Yes, you are. A lot of factors, a lot of ifs. But if done properly, it is a pretty good marker once again of renal function. Now because of that slight secretion, we just said that it would be greater than GFR. Understand that point. Do not just breeze through that. 06:46 GFR is equivalent to filtration. Clearance is what you are actually evacuating from your body. Because of slight secretion, I repeat once again that creatinine has greater clearance than GFR. Used as an approximation of GFR. What is CrCl? Creatinine clearance. How do you assess this test? This is not the blood test. This is the one in which you are measuring how much creatinine is actually being cleared.
About the Lecture
The lecture Basics of Creatinine by Carlo Raj, MD is from the course Renal Diagnostics.
Included Quiz Questions
Which of the following statements correctly describes the process of secretion in the kidney?
- Movement into the tubular lumen.
- Movement away from the tubular lumen.
- Movement into the tubulointerstitium.
- Movement into the interstitium.
- Movement into the blood.
Which of the following can accurately measure creatinine clearance?
- 24 hour urine sample
- Arterial blood sample
- Renal venous blood sample
- 22 hour urine sample
- Venous blood sample
Which of the following statements is correct regarding the metabolism of creatinine in the kidney?
- It is freely filtered, slightly secreted and not reabsorbed.
- It is freely filtered, and neither secreted nor reabsorbed.
- It is freely filtered, fully secreted, and partially reabsorbed.
- It is partially filtered, fully secreted, and not reabsorbed.
- It is freely filtered, slightly secreted, and completely reabsorbed.
What is the normal range of serum creatinine?
- 0.6-1.2 mg/dL
- 1.2-2.4 mg/dL
- 0.4-1.2 mg/dL
- 0.4-1.5 mg/dL
- 0.6-0.8 mg/dL
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
1 customer review without text
1 user review without text