Playlist
Show Playlist
Hide Playlist
Auscultation of the Heart: Diastolic Murmurs
-
Reference List Physical Examination.pdf
-
Download Lecture Overview
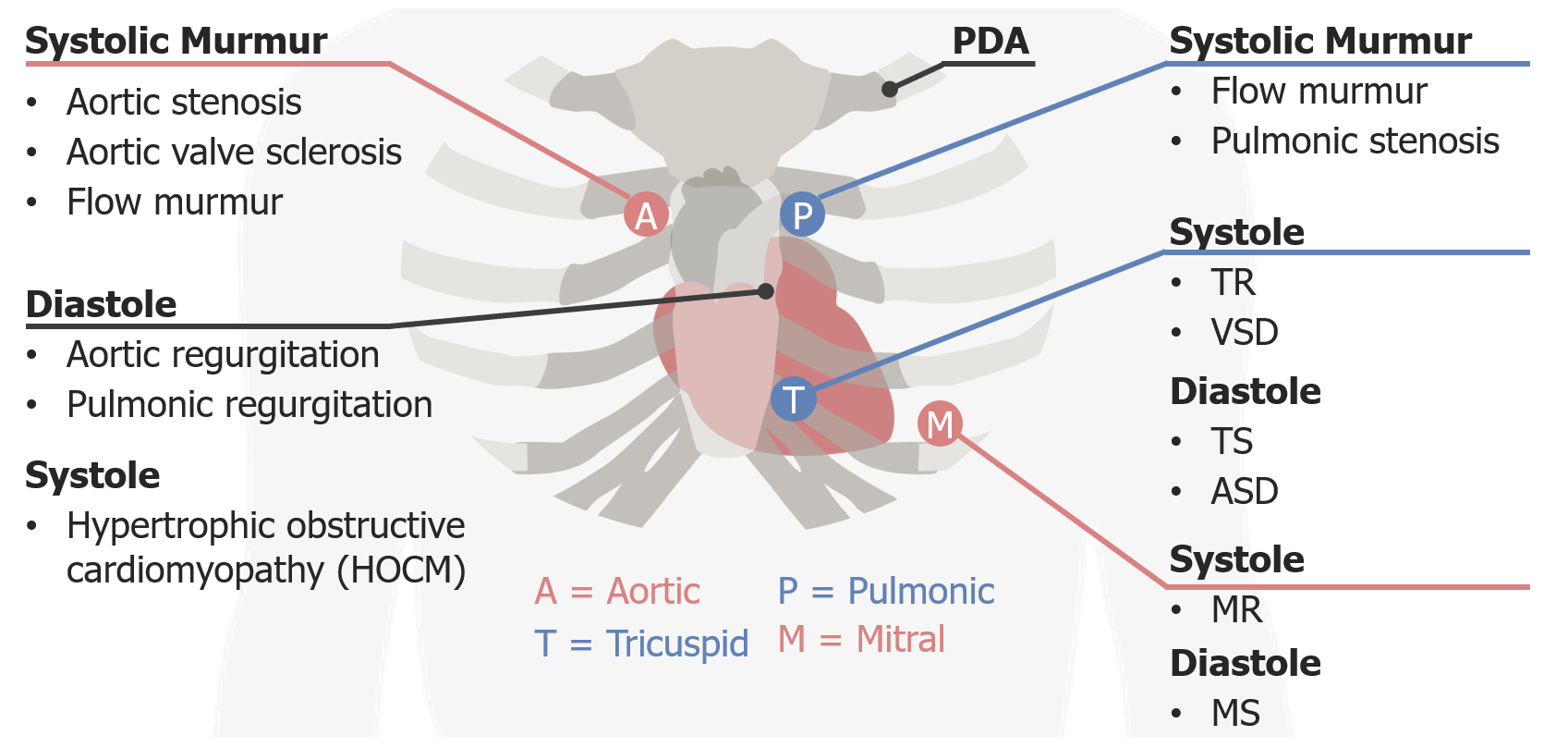
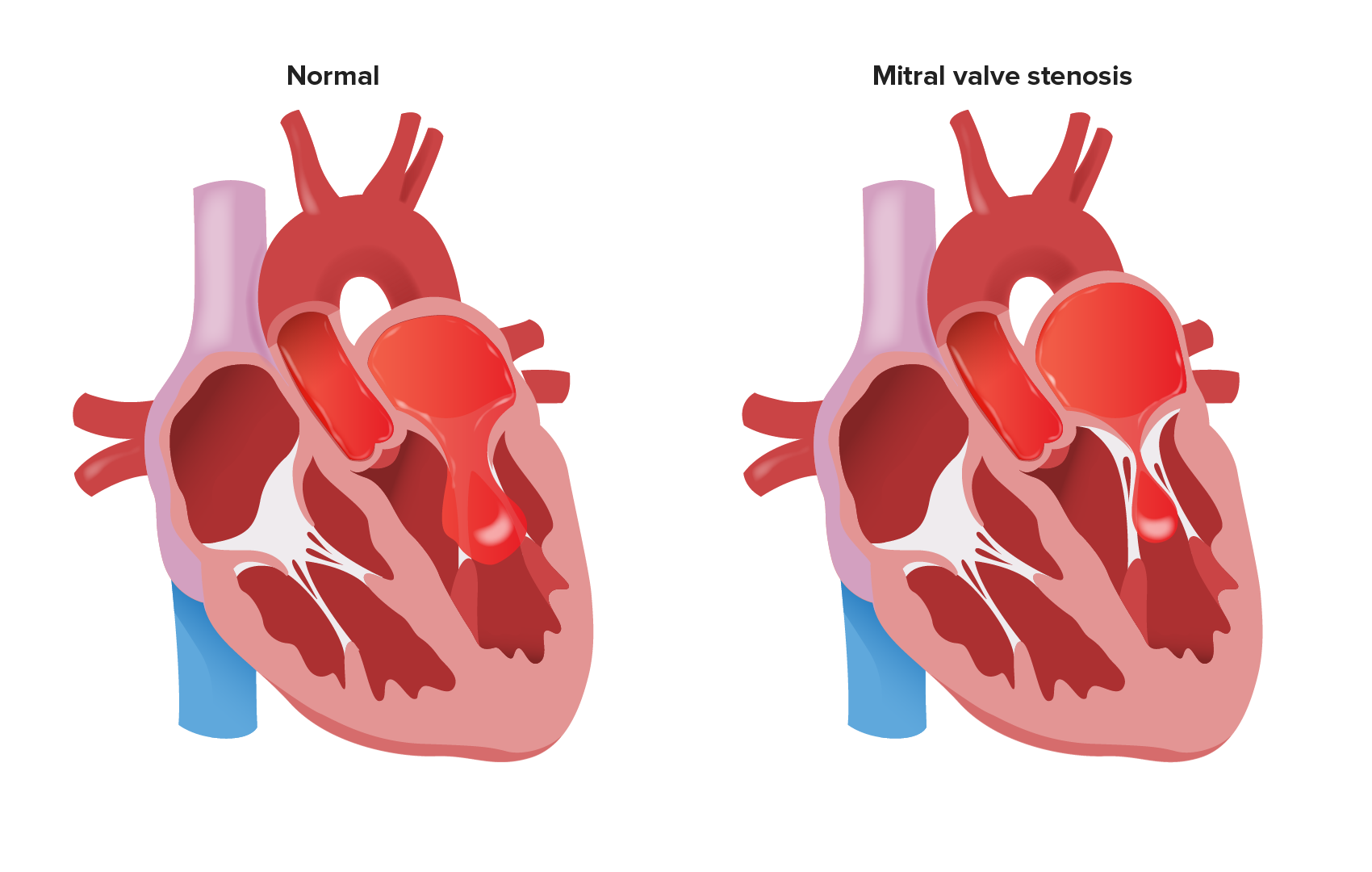
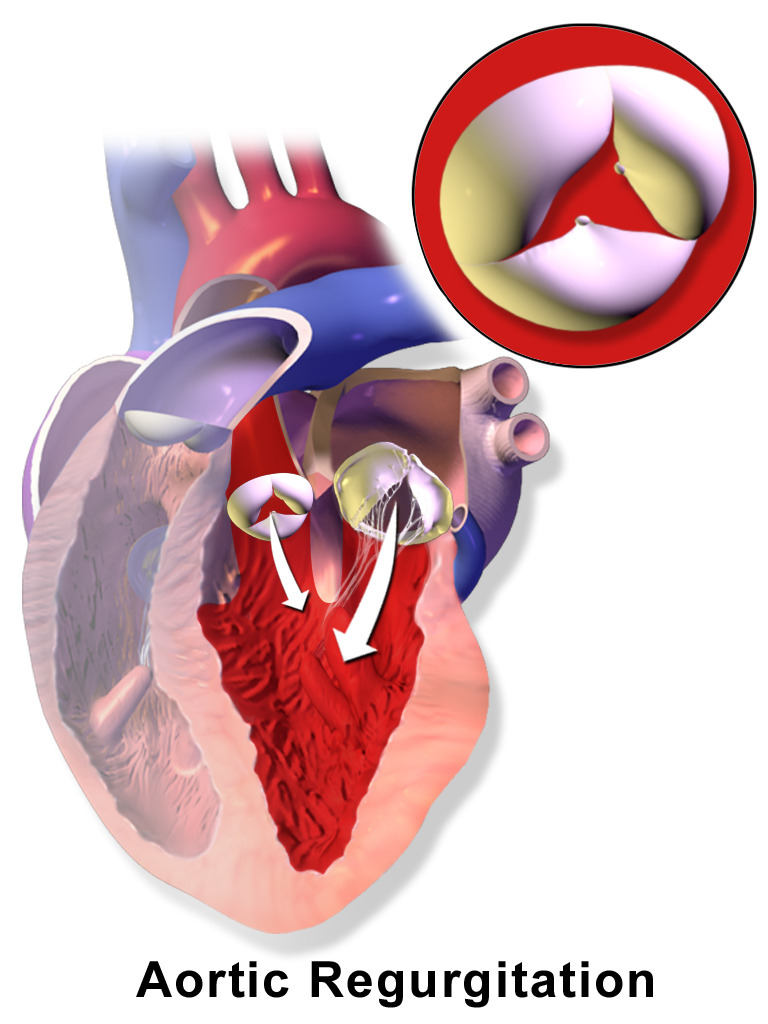
00:01 So, as I just said, diastolic murmurs are always worth investigating. 00:06 And the two ones we're going to look at are aortic regurgitation or also known as aortic insufficiency, and mitral stenosis. 00:13 Aortic insufficiency is a remarkable cardiac valve problem that has a variety of different manifestations with dozens of different eponymous findings that have been described. 00:26 I'm really going to focus on some of the cardinal features of aortic regurgitation and let's start off with my little acronym, LISPT. 00:33 So location. 00:34 The best place to listen for aortic regurgitation is going to be the tricuspid area, it's actually somewhat between the pulmonic and tricuspid areas where you'll hear this diastolic murmur. 00:44 Intensity. 00:45 This is a soft murmur and that's why going back in the beginning of this lecture, I talked about the importance of listening deliberately to the heart sounds, to systole and diastole. 00:56 Many is the case where I've been with the resident or student who speaks volumes about the systolic murmur that they heard but they completely neglect to pick up the diastolic murmur because they were so focused on just hearing the systolic murmur, so it's very important to really focus on that period between S2 and S1 which is so often neglected. 01:17 So the intensity of this murmur is going to be quite, certainly the more intense it is, the more that does correlate with the severity of the insufficiency. 01:27 Shape and pitch. 01:29 So this is also a high pitch sound. It tends to be decrescendo, purely decrescendo. 01:35 The classic onomatopoeia phrasing for this one is [making a sound], so it's starting off relatively high, maybe a little bit in the early peak and then going down again, [making a sound] but it's going to be a lot softer, it's very subtle, you really have to pay attention to find it -- the pitch is high. 01:59 And then in terms of the timing. 02:01 It tends to occur immediately as a diastole's beginning cuz remember, when the left ventricle contracts, it immediately closes the mitral valve and the tricuspid valve, that's S1, and then as soon as the aortic valve closes, which is the beginning of S2, it's not fully closing, what's happening is that blood is now starting to regurgitate back into the left ventricle, that's the cardinal feature of aortic insufficiency, is blood going backwards. 02:30 So there's this constant to and fro, to and fro motion to aortic regurgitation. 02:37 It tends to not radiate though sometimes you can hear what's called an Austin Flint murmur here at the apex which is the sound of that regurgitating jet of blood hitting the left ventricular apex. 02:49 The other important features about aortic regurgitation are starting with the pulse pressure. 02:56 So when the left ventricle contracts, that's what maintains your systolic blood pressure, blood contracts, there's this huge surge of blood out into my extremities, where someone's got a blood pressure cuff on and you detect that Korotkoff knocking sound of blood shooting past or shooting underneath my blood pressure cuff, that's the systolic impulse itself. 03:17 But, of course, from one systolic impulse to the next, it's not as if our blood pressure collapses, right? There's our diastolic pressure, there's this pressure that's maintained during the space between those systolic contractions, that's your diastolic pressure and the thing that maintains that pressure, so that we aren't just constantly losing consciousness between every beat of our heart, is the fact that our aorta has recoil. 03:43 When blood shoots to the aorta, it dilates, the valves close, and then the aorta has elastic recoil that then constricts around that huge jet of blood which then is maintaining the pressure downstream during diastole. 03:58 The trouble is that once systole happens and the valve closes, when the aortic arch recoils, if the valve holding it together is not functioning, the aorta recoils and the blood is going now backwards back into the heart. 04:15 Any valve systems requires valves that close tightly and if the aortic valve is not closing tightly, blood's going to go on both ways, some of them are going to go forward, but a lot of it is going backward. 04:25 Because of that, we find a very clear manifestation of that simply by checking somebody's blood pressure, you have a high systole and a very low diastole, that's called your pulse pressure, it's the difference between your systolic blood pressure and your diastolic blood pressure. 04:40 So let's say that our patient for example here had a blood pressure of 130/50, so 130 being the systolic, 50 being the diastolic, it's the difference between them that tells us what the pulse pressure is and again, that's that concept of the 130 is your what are happening during systole, which is your left ventricular impulse, and the 50 is your diastolic pressure being maintained by that aortic recoil with a competent aortic valve. 05:07 Somebody's pulse pressure if it's 80, the difference between 130 and 50 has a very significant prognostic sign suggestive of aortic regurgitation and it's something which you just wouldn't normally see for otherwise healthy people. 05:21 So that's one feature, is the pulse pressure. 05:24 The other feature is, I made mention of all those eponymous findings in aortic regurgitation, all of them are ultimately derived from this idea that blood is being forcefully ejected and then it's flowing right back again, and those manifestation of that that you can find. 05:39 In a patient who has severe aortic insufficiency, you may find that on their hands, you can see that there's a little bit of pinkness on the fingernails there. 05:47 In someone who has these widely, wide excursions of systolic and diastolic pressures, you may actually see that that red to white border there, moves out with every pulsation of his heart, those are called Quincke's pulses, you'll see this to and fro motion happening right there on the nail bed. 06:04 You may see that a patient has got severe disease, may even have their heart, their head pumping up and down like this with each pulsation of their heart and that's called De Musset's sign. 06:14 You may find if you open up their mouth and look in the back at their uvula, that the uvula itself may even have a little bit of a pulsation and that's called Muller's sign. 06:23 There are a dozen of these kinds of little esoteric findings that you could see with aortic regurgitation, they're all basically just describing different manifestations of the exact same process. 06:35 Along the same lines, you can auscultate the femoral artery or other arteries and you'll find that if you put the bell of your -- the diaphragm of your stethoscope on the artery, you'll hear blood rushing underneath your stethoscope and then you'll hear it rushing backwards again, blood is literally going backwards in your circulation, they're all pointing to the same thing. 06:57 Now, importantly, I don't want to highlight those particular eponyms because while they are interesting and they certainly tell us about the pathophysiology of the disease, the reality is that the sensitivity and specificity for those findings is so poor that we really can't hang our hat on whether those findings are present or absent. 07:18 Instead I want you to focus on the pulse pressure, the characteristic finding of an early diastolic decrescendo murmur, and then one last important feature, you can imagine that if all that blood is going out and going back in again, your left ventricle is having to do twice the work, right? Not only using trying to pump the blood that came from the left atrium there, it's now going to pump the blood that fell back in from the aortic arch into there so that blood is working overtime and you're going to hear an S3, a third heart sound we talked about in the beginning of the lecture, because it's almost as if the heart is in failure, it's so overloaded, there's such increase diastolic filling pressures, that you're going to hear an S3. 07:59 The presence of the 3rd heart sound does serve as a highlighting good ratio for the presence of aortic insufficiency in the setting of these other features. 08:08 Alright, so that's aortic regurgitation. 08:10 One last diastolic murmur and this is the murmur of mitral stenosis. 08:15 Now fortunately, we don't see a lot of mitral stenosis anymore ever since the advent of antibiotics that are being distributed all over the world to prevent rheumatic fever cuz basically, mitral stenosis is almost every time, unless it's surgical or a few other rare birds, it's caused by progressive closure and stenosis of the mitral valve in the setting of rheumatic heart disease. 08:39 The murmur of mitral stenosis which I myself have only heard a handful of times is low, it is again diastolic, we are going to hear it over here at the apex, so again location apex, intensity its fairly quiet though depending upon how loud is that that does correlate with the disease, and then the shape and the pitch, this sound is described as a rumble or even the growling of a dog so it sounds like this [making a sound] very low in pitch, guttural, but fairly holodiastolic. 09:16 So that's the murmur of mitral stenosis and with that, I think we've covered all the different murmurs that we're going to potentially hear and now we should move on to start talking about a few specific cardiac conditions that are non-valvular in nature.
About the Lecture
The lecture Auscultation of the Heart: Diastolic Murmurs by Stephen Holt, MD, MS is from the course Examination of Cardiovascular and Respiratory System.
Included Quiz Questions
What are the cardinal features of a murmur related to aortic insufficiency?
- Located at the left sternal border, diastolic decrescendo murmur, sometimes associated with an S3 sound
- Located at the right upper sternal border, holosystolic, may radiate to the right carotid area
- Located anywhere in the chest, heard during diastole between S1 and S2
- Located at the apex, heard during systole, causes increased pulse pressure
- Located at the left sternal border, associated with an S4 sound and decreased pulse pressure
What are the cardinal features of a murmur related to mitral stenosis?
- Located at the apex, heard during diastole, described as a low-pitched rumble
- Located at the apex, heard during systole, causes increased pulse pressure
- Located at the left sternal border, associated with an S4 sound and decreased pulse pressure
- Located at the right upper sternal border, holosystolic, may radiate to the right carotid area
- Located at the left sternal border, diastolic decrescendo murmur, sometimes associated with an S3 sound
What is pulse pressure?
- It is the difference between systolic and diastolic blood pressure.
- It is the pressure of blood ejected during systole.
- It is the pressure of peripheral vascular resistance during diastole.
- It is the pressure of blood ejected during diastole.
- It is the pressure of peripheral vascular resistance during systole.
Which valvular heart disease is associated with rhythmic head bobbing, pulsation in the uvula, and Quincke's pulse?
- Aortic regurgitation
- Mitral regurgitation
- Mitral stenosis
- Aortic stenosis
- Tricuspid regurgitation
Which valvular heart disease is associated with increased pulse pressure?
- Aortic regurgitation
- Mitral regurgitation
- Tricuspid regurgitation
- Aortic stenosis
- Mitral stenosis
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
2 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Love this lesson! Dr. Holt is a true master of the cardiac exam.
1 customer review without text
1 user review without text