Playlist
Show Playlist
Hide Playlist
Atherosclerotic Cardiovascular Disease: Management
-
Slides AtheroscleroticCardiovascularDisease ChronicCare.pdf
-
Download Lecture Overview
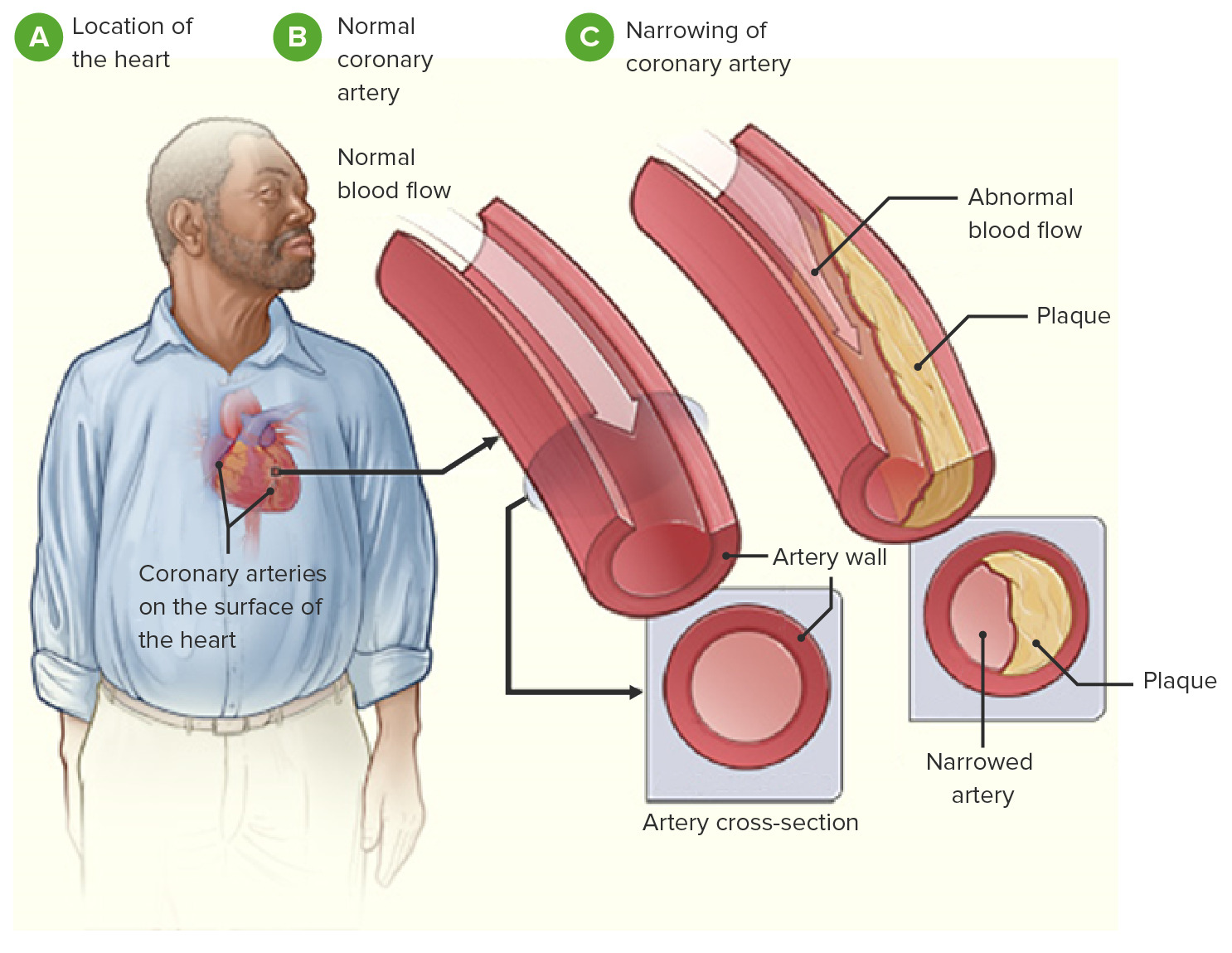
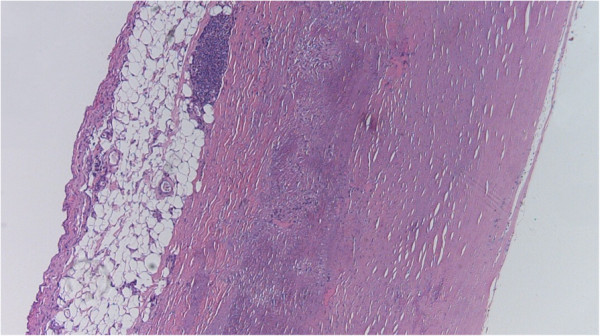
00:01 So, the patient is diagnosed unfortunately with ST elevation myocardial infarction. 00:06 And while he is in the hospital, he gets good evidence-based treatment, gets a percutaneous intervention and, lo and behold, they put in two coronary stents. 00:16 All of the following medication should be initiated at discharge except for remember, this is an except question. 00:22 So, everything except, A, aspirin, clopidogrel or both; B, a beta blocker; C, a diuretic; or D, a statin. 00:31 Which do you think should not be initiated in this patient? A diuretic. 00:37 The other drugs are more or less necessary. 00:39 And let’s go through them. 00:41 So, aspirin is standard antiplatelet therapy. 00:44 Certainly should be included for patients with a history of symptomatic cardiovascular disease or any cardiovascular event. 00:52 There is not a difference in efficacy. 00:55 81 mg to 325 mg. 00:59 But do realize the higher you increase your dose of aspirin, the higher risk of hemorrhage, and we’re talking about a drug that patients are going to be taking over years. 01:06 So, it doesn't seem like just one aspirin a day should promote a greater rate risk of particularly gastrointestinal bleeding, but it does over time. 01:14 Clopidogrel is often employed after stent placement. 01:18 And particularly for patients with stroke, it's slightly superior to aspirin preventing recurrent strokes. 01:25 So, if a patient just has a history of stroke, I'll prefer them on a clopidogrel versus aspirin. 01:32 And the combination of aspirin and clopidogrel is frequently used and has been associated with improved effects after stent placement. 01:40 Usually that's for approximately one year. 01:43 However, do understand, at the same time, that using two antiplatelet agents together is associated with a higher risk for bleeding. 01:50 So, that's part of the balance. 01:52 It may be why it’s not a great idea to continue patients forever on both drugs because they will have higher risk of bleeding. 02:02 In terms of other drugs that are recommended for stable atherosclerotic cardiovascular disease, high-intensity statins, definitely helpful. 02:10 One of the questions that comes up is, well, what about tolerability if I'm using high-intensity statins. 02:17 There really isn't a strong difference in terms of discontinuation rates of moderate verse high-intensity statins, so go for the high-intensity statins. 02:26 Your patients will have a reduced risk of other cardiovascular events if you can get them on a high-intensity statin. 02:33 Beta blockers as well should be universal. 02:36 So, it’s a first line anti-hypertension agent among these patients and a significant reduction in mortality. 02:42 The main side effect is bradycardia, and so that’s something to watch out for and you might need to titrate your dose, but most patients tolerate beta blockers very well. 02:53 And if it’s beta-1 selective, you can even use it in patients with asthma and COPD, although with some caution. 03:00 Whereas an ACE inhibitor or an angiotensin receptor blocker, ACEI or ARB, are second line for hypertension and they probably are also associated with some benefit in these patients with cardiovascular disease beyond their blood pressure. 03:13 Nitrates are really a backup as an anti-anginal beta blocker, so are your number one anti-anginal drug because they, one, are effective at treating angina, but secondarily they promote better mortality effects versus nitrates. 03:32 But for patients with breakthrough type angina, nitrates can be effective as well. 03:39 So, that's really what I want to describe today with regard to existing cardiovascular disease. 03:46 I think the main take-home points for your patients for your exam are maintaining that stable of drugs. 03:53 We’re talking about three or four agents for all patients who’ve had a history of either cardiac revascularization procedures or some kind of cardiovascular event. 04:05 So, those really should be lifelong treatments. 04:07 So, think about them and providing them in the long term and make sure patients are thinking about them as well and they’re enlisted and empowered in their plan of care. 04:16 Thanks.
About the Lecture
The lecture Atherosclerotic Cardiovascular Disease: Management by Charles Vega, MD is from the course Chronic Care.
Included Quiz Questions
Which of the following drug categories have anti-anginal effects?
- Beta-blockers
- Angiotensin-converting enzyme inhibitors
- Antiplatelet drugs
- Anticoagulants
- Loop diuretics
Which of the following drugs is superior for the secondary prevention of ischemic stroke?
- Clopidogrel
- Aspirin
- Unfractionated heparin
- Beta-blockers
- Nitrates
What is the typical duration of dual antiplatelet therapy after placement of intracoronary stents in stable patients?
- 6 months to 1 year
- 1-2 years
- Lifelong
- 2-3 years
- 3–6 months
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |