Playlist
Show Playlist
Hide Playlist
Acute Nephritic Syndrome: Fundamentals
-
Slides Nephritic Syndrome.pdf
-
Reference List Nephrology.pdf
-
Download Lecture Overview
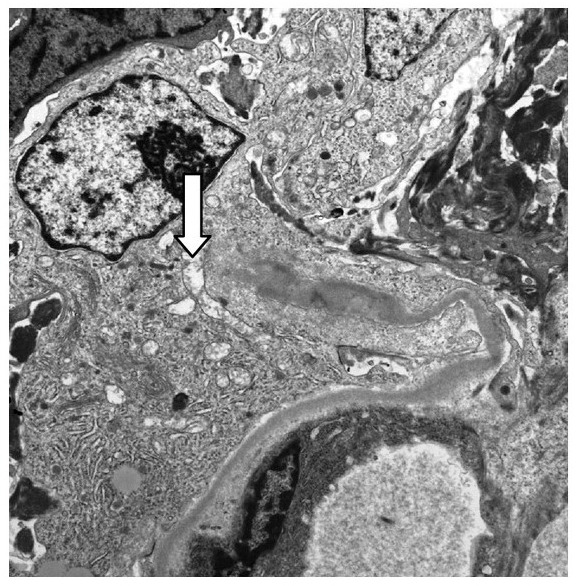
00:01 Hello, and welcome back to the nephrology curriculum. 00:03 Today, we're gonna be talking about nephritic syndromes. 00:07 Nephritic syndromes are part of the glomerular diseases and I can say as a nephrologist, they're probably one of the most exciting aspects of my job. 00:14 So, when we think about acute nephritic syndrome, it's characterized by 5 different components from the clinical standpoint. 00:22 This includes hematuria of glomerular origin. 00:26 That means that when I look at the urine underneath the microscope, I can see what we call dysmorphic red blood cells. 00:33 That means that the red blood cell has a funny shape to it. 00:36 So, if you look at the normal red blood cell, you can see that it's beautifully shaped, circular in appearance. 00:41 But when you see a dysmorphic red blood cell, there are these little blebs all over the membrane and sometimes, they even take on a Mickey Mouse appearance. 00:50 It's not uncommon for us to call them Mickey Mouse cells. 00:52 We can also see red blood cell cast and that means that these red blood cells collect in the tubule, they bind with that Tamm-Horsfall protein, and they form this beautiful cylindrical cast full of red blood cells with just a slight reddish hue. 01:07 We also see proteinuria in our nephritic patients and that proteinuria is usually between 150 mg to 3.5 g per day. 01:17 So, what we would term sub-nephrotic. 01:20 Again, we can have some patients who have greater than 3.5 g of proteinuria even though they have nephritic syndrome and these are typically patients who have overlap syndromes. 01:31 That includes membranoproliferative glomerulonephritis and lupus nephritis which we're gonna be talking about today. 01:37 Azotemia also characterizes nephritic syndrome. 01:41 That means we have an elevated blood urea nitrogen, typically that BUN-to-creatinine ratio is greater than 15. 01:48 And oliguria, our patients are classically oliguric, meaning that they make less than 500 mL of urine per day. 01:57 And finally, hypertension. 01:59 Patients who have acute nephritic syndrome will manifest with higher blood pressures. 02:03 This is typically because they are volume overloaded. 02:06 These patients are retaining sodium and it's interesting because they actually have suppression of the renin-angio-aldo system and essentially, they have an increase in the sodium-potassium ATPase at that principal cell that's responsible for that sodium uptake leading to volume overload. 02:24 So, when we think about the different types of disorders that manifest as acute nephritic syndrome, they include membranoproliferative glomerulonephritis. 02:33 It's a little bit difficult to say so we like to abbreviate that as MPGN. 02:38 There's IgA nephropathy, post-infectious glomerulonephritis and some people refer to that as infection-associated glomerulonephritis. 02:48 Lupus nephritis and then there are the rapidly progressive glomerulonephritis. 02:54 And what that means is that patients, clinically, have a rapid deterioration in their renal function and morphologically, when we biopsy these patients, on pathology, we see something called necrosis and crescents. 03:09 These include anti-GBM disease, Goodpasture syndrome if it includes both lung and kidney. 03:15 The immune-complex diseases that I just spoke about. 03:19 That includes lupus, IgA, post-infectious, and MPGN. 03:24 If they manifest with a rapid deterioration in renal function and morphologically, they have crescents and necrosis on pathology, those patients would be considered in RPGN. 03:36 And finally, the Pauci-immune glomerulonephritis and that includes our ANCA-associated vasculitis.
About the Lecture
The lecture Acute Nephritic Syndrome: Fundamentals by Amy Sussman, MD is from the course Nephritic Syndrome.
Included Quiz Questions
What best defines oliguria?
- < 500 mL of urine per day
- > 500 mL of urine per day
- < 100 mL of urine per day
- > 1,000 mL of urine per day
- < 50 mL of urine per day
Which of the following may present with clinical features of both nephrotic and nephritic syndromes?
- Membranoproliferative glomerulonephritis
- Diabetic nephropathy
- Membranous nephropathy
- Minimal change disease
- Poststreptococcal glomerulonephritis
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |