Playlist
Show Playlist
Hide Playlist
Abdominal Aortic Aneurysm: Examination and Diagnosis
-
Slides Abdominal aortic aneurysm Special Surgery.pdf
-
Download Lecture Overview
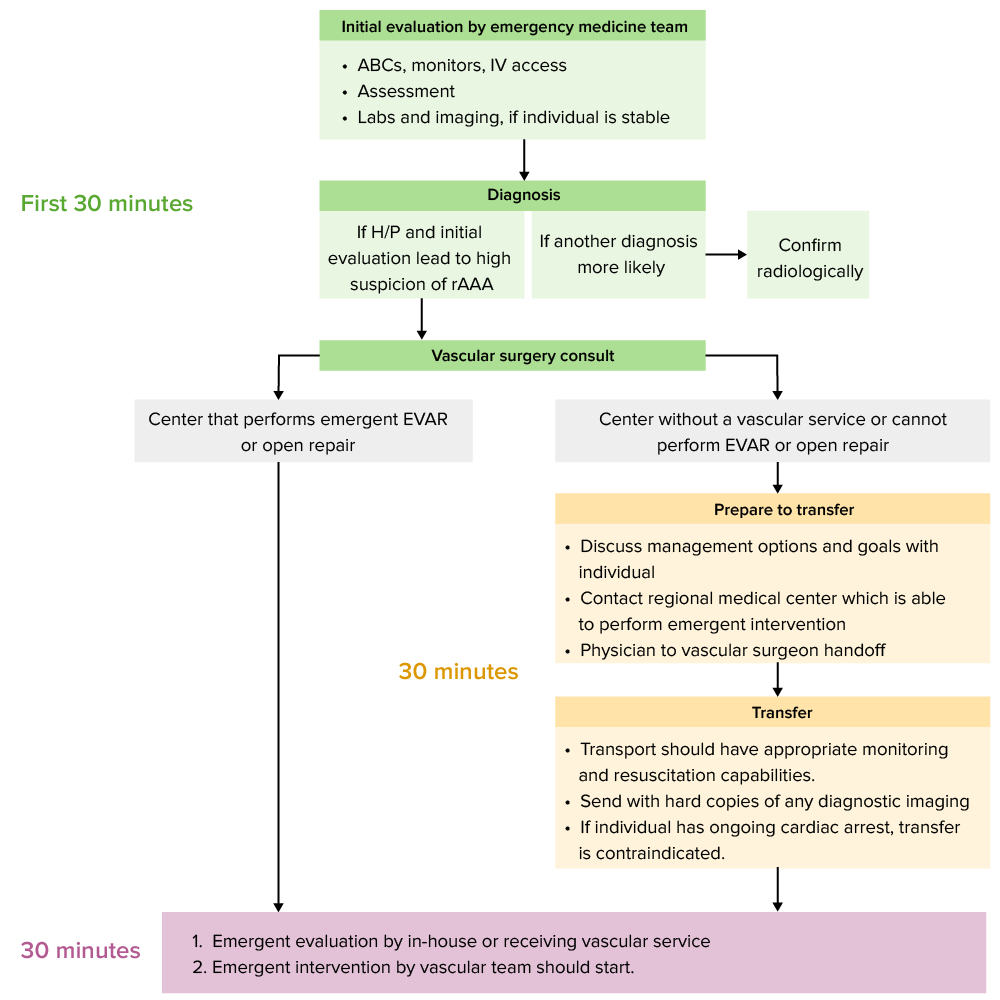
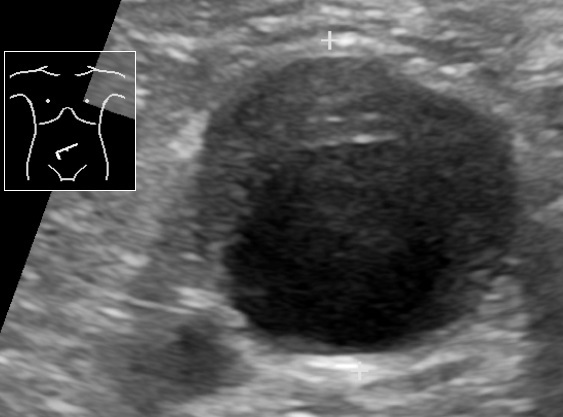
00:01 Let me pose a question to you. 00:02 What is the classic presentation for a patient with impending AAA rupture? I'll give you a second to think about this. 00:12 That's right, severe abdominal pain radiating to the back, and potentially a pulsatile mass. 00:18 Now, with the increase of obesity, our patients are more and more difficult to diagnose in terms of pulsatile masses. 00:26 So don't count on that as a finding. 00:31 Laboratory values are unlikely to be of any help to you. 00:34 Even in the setting of a massive bleed from an aortic rupture, the H&H of the hemoglobin and hematocrit may not have changed. 00:43 Now, let's move on to a useful imaging or diagnostic studies. 00:47 Ultrasound is fairly standard. 00:50 Introduces no radiation, and it's easy to follow the patient up. 00:54 However, as with any ultrasound, it is operated dependent in terms of the results that you obtained. 01:02 Here on this image, you see an ultrasound with velocities. 01:05 The velocities are at the peaks and valleys. 01:08 Remember I said earlier, if there is stenotic flow, the velocities tend to be higher. 01:14 In the right upper quadrant of that image, you see an ultrasound with a large cystic lesion. 01:20 How do I know it's cystic or fluid filled? Because it's anechoic, completely dark. 01:25 This is in fact a demonstration of aneurysmic aortic sac. 01:30 Cross sectional imaging is increasingly used for CAT for abdominal aortic aneurysm diagnosis and follow up. 01:38 In this image, we not only see aneurysm but we also see a false lumen. 01:46 You see the actual calcified aneurysm in the center of the image. 01:51 This patient also has fluid around this abdominal aorta. 01:55 Is this patient and impending rupture? Have about angiography? We typically don't think of using angiography as standard diagnostic tool for AAA. 02:06 And the reason is because we're not only interested in the intraluminal filling. 02:10 Remember, if you perform an invasive angiography, the information you're gathering is actually only information on the inside of the lumen. 02:19 For abdominal aortic aneurysms, cross sectional imaging is far more helpful. 02:25 And as a reminder, non-invasive angiography is obtained by multi detector slices are far more accurate these days. 02:34 Here's a neat 3D reconstruction based on cross sectional imaging. 02:38 The AAA is clearly labeled for blue in red. 02:41 Know that proximal and distal to this region, there are some tortuosity but the diameter of those vessels are largely normal.
About the Lecture
The lecture Abdominal Aortic Aneurysm: Examination and Diagnosis by Kevin Pei, MD is from the course Special Surgery.
Included Quiz Questions
Severe abdominal pain and a pulsatile mass in the abdomen may be an indication of which of the given conditions?
- Ruptured abdominal aortic aneurysm
- Ruptured aortic root aneurysm
- Thoracoabdominal aortic aneurysm
- Aortic root aneurysm
- Unruptured abdominal aortic aneurysm
All of the following are diagnostic imaging tools for abdominal aortic aneurysm EXCEPT?
- Plain radiographs
- Ultrasonography
- CT scan
- MRI
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |