Playlist
Show Playlist
Hide Playlist
Abdominal Aortic Aneurysm and Thoracic Aortic Aneurysm
-
Slides Aortic Disease.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
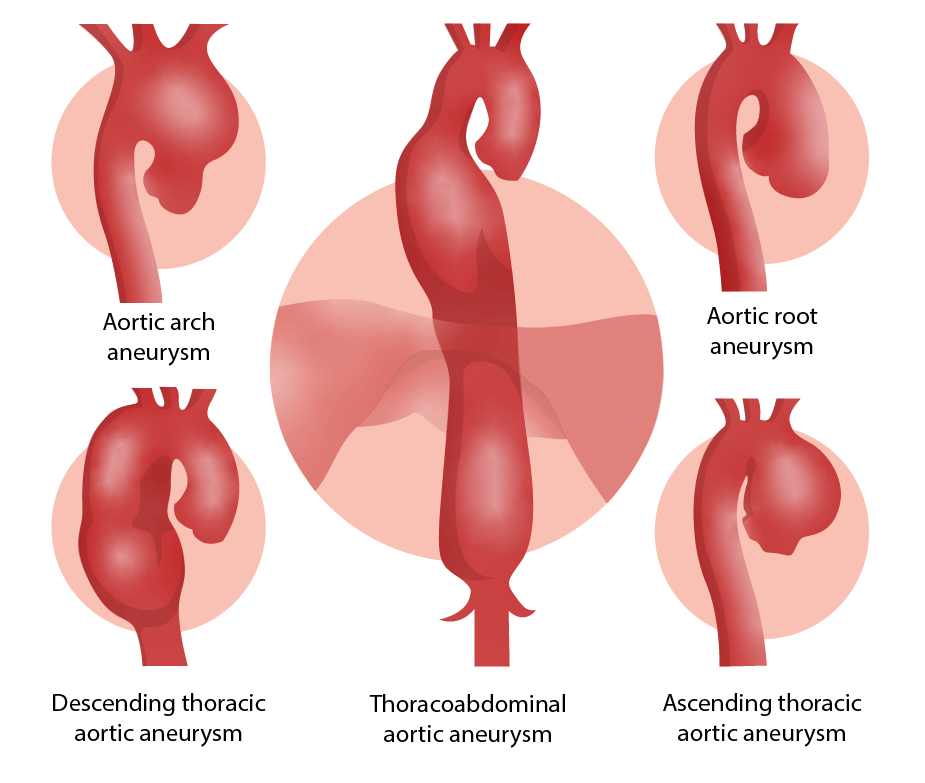
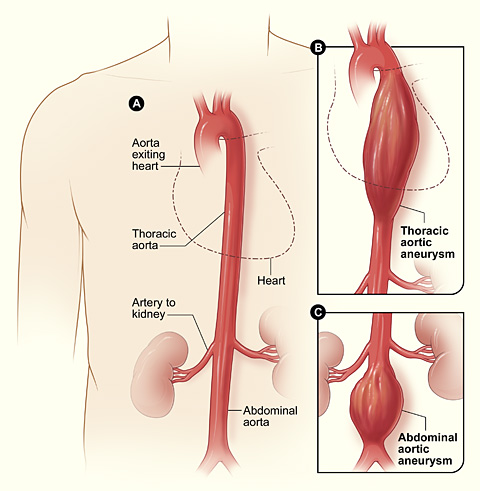
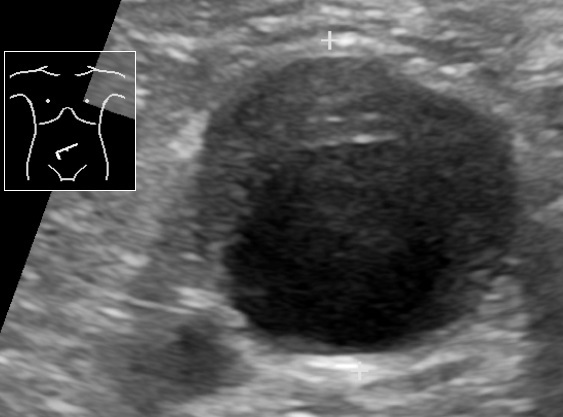
00:01 So who gets abdominal aortic aneurysm? So we have aneurysms that are going to affect various parts of the aorta from the ascending aorta, the thoracic aorta, descending aorta, and infrarenal abdominal aorta. 00:14 So this is abdominal aortic aneurysm or AAA, much more common in men than in women, much more common in smokers. 00:23 So smoking probably has some effect on activating the inflammatory cells that give rise to AAA. 00:31 The incidence is about 3% in individuals who are 65-75 years old, so it's reasonably common. 00:38 In fact, if you do a careful exam on your geriatric population, you will find this not infrequently. 00:46 The incidence goes up and the incidence is shifted to younger years. 00:52 It's people who are smokers, so 4.3% of smokers who are a decade or so younger. 00:59 Atherosclerosis is probably the initial driving force for abdominal aortic aneurysms. 01:04 But it's also the nature of the inflammatory cells and what they're making that is breaking down elastic tissue and causing defective collagen synthesis. 01:13 Abdominal aortic aneurysms typically occur in the infrarenal aorta, that's actually because there is an additional component of turbulence. 01:22 So the same factors overall causing atherosclerosis everywhere within the aorta. 01:27 But in the infrarenal aorta kind of there, and into the iliac bifurcations, there's greater turbulence because we have blood coming and then hitting that bifurcation. 01:37 So in that zone is where we tend to see the worst atherosclerosis in the aorta, but also where the abdominal aortic aneurysms occur. 01:46 Here's an example. 01:47 So we have on the left hand side an aorta, near the top of the picture would be the patient's chest, and ultimately, their head towards the bottom is the bifurcation of the iliacs into the legs. 01:59 And you see in the region below the level of the renal arteries, there is a somewhat dilated fusiform aneurysm that here is filled up with blood at higher magnification. 02:11 Why is that happening? Well, that's happening because we have an abnormal flow in this location. 02:16 We have weakened the wall, it's dilated. 02:19 And now we have that bifurcation too, where we have turbulence, a combination of the dilated wall, abnormal flow, turbulence is going to give us thrombus formation. 02:29 So that can also be a cause of occlusion of the vasculature in that location. 02:36 This is just giving you a sense of this on an angiography CT. 02:40 So the contrast material is bright white and the arrow is pointing to the abdominal aorta. 02:48 The area that is bright white is the lumen. 02:51 So that is the contrast material within the lumen but you see a slight you see a darker region of grey, above and to the left of that brightness that represents the actual outline of the aorta because it's dilated, but now that has been filled in with a blood clot. 03:12 So there is no contrast material in there. 03:14 That's blood clot in a dilated aortic aneurysm. 03:20 Other causes of abdominal aortic aneurysms rarely 5-10% of the time are inflammatory aneurysms. 03:27 This is much more driven by inflammation, and typically occurs in a much younger patient population. 03:37 Patients with inflammatory aneurysms tend to have elevated inflammatory markers, and may present with relatively acute onset of back pain. 03:47 There is also immunoglobulin G4/ IgG4-related aortic disease, and this is associated with high plasma levels of IgG4 and high levels of plasma cells expressing IgG4 within tissue fibrosis around the aorta. 04:03 This can affect not only the abdominal aorta but other areas within the aorta and also can affect the pancreas, the biliary system, salivary glands amongst others. 04:14 So IgG4-related disease is a different, an interesting entity that is discussed in other talks. 04:20 If you want to scan around on the Lecturio site, you can find it because I talked about it. 04:26 Then there's mycotic aneurysms. 04:28 These are lesions that are infected by circulating microorganisms that have gone in through the vasa vasorum and have now caused local destruction of the wall leading to aneurysm formation. 04:40 Signs, symptoms, and complications. 04:42 So again, this is showing you a reconstruction of an angiography study where we have an abdominal aortic aneurysm that's indicated by the white box and it's below the renal arteries above the bifurcation of the aorta. 04:56 That's the classic location. 04:58 This patient also has aneurysms that involve the smaller iliac arteries. 05:03 Those are very dilated, they're not the normal calibre. 05:08 Commonly, AAAs are asymptomatic. 05:12 That's why you have to do a very careful exam on your geriatric population to actually find them. 05:17 But if they're going to be symptomatic the kinds of symptoms that they will have is that you can have frank rupture. 05:23 These things can get big enough, and the walls can become defective enough, thin enough that you actually formally rupture. 05:30 It usually leads to exsanguination with hemoperitoneum. 05:34 You can have obstruction of vessels branching off the aorta as a result of the dilation, the expansion and superimposed thrombosis. 05:44 In that thrombosis, you can also have things that fragment often embolize into the distal extremities, for example. 05:52 You can get compression of the ureters so that you get (hydro)nephrosis of the kidneys or you can even erode into the vertebrae as this pulsatile mass expands and expands and expands and rubs up against the vertebral bodies. 06:07 The risk of rupture, when aneurysms are less than 5 cm is 1% per year. 06:13 Even so, that 5% limit is where we will do either a surgical intervention or we will do put in intravascular stents to keep the aneurysm from expanding and potentially rupturing. 06:27 The risk of rupture is greater than 10% if it gets to 5-6 cm. 06:32 And if it gets larger than 6 cm, 1 out of 4 patients will have a rupture each year. 06:39 That's pretty substantial. 06:40 And when patients rupture, a AAA, they usually die as a result of exsanguination. 06:48 Alright, that's AAA's, which overall are going to be more common than thoracic aortic aneurysms. 06:56 Having said that, we're going to talk about thoracic aortic aneurysms because they're important to recognize them, we understand some of the etiology as we discussed previously. 07:04 Hypertension is going to be the most common cause in most developed countries for thoracic aortic aneurysms and this can be ascending aorta. 07:12 This could be over the arch, this could be the intrathoracic descending aorta. 07:18 All of those. 07:18 So hypertension is going to be most common, and that's again because we are compromising the lumina, the vessel lumen of those vessels of the vasa vasorum. 07:29 Marfan Syndrome will be another cause of thoracic aortic aneurysms usually in families. 07:35 But we can have spontaneous mutations of the fibrillin gene, Loeys-Dietz syndrome again because of defective or abnormal TGF-beta, and TGF-beta receptor signalling. 07:45 Syphilis is a relatively uncommon cause at least in developed countries for thoracic aortic aneurysms. 07:52 But because the syphilitic organisms the Treponema pallidum. 07:56 like to infect the vessels of the vasa vasorum of the arch of the aorta. 08:02 Iit is a cause of thoracic aortic aneurysms. 08:05 We tend not to see syphilitic aortitis and syphilitic aneurisms anywhere below the diaphragm. 08:12 So how can this present in terms of symptomatology. 08:16 So many thoracic aortic aneurysms may be totally asymptomatic. 08:21 Okay, that is just a given. 08:24 They may have respiratory difficulty or stridor or dyspnea. 08:28 Because of compression of the trachea or some of the bronchi. 08:34 Just as the thoracic aneurysm expands, they may also compress pulmonary vessels. 08:40 So you may have a degree of dyspnea associated with extrinsic compression by enlarging aneurysm. 08:47 They may have difficulty swallowing dysphagia. 08:49 This has to do with the innervation of the esophagus and also the compression external compression of the esophagus. 08:57 So they may have dysphagia. 08:59 A persistent cough again is because of irritation of the recurrent laryngeal nerve, and they may even have hiccups because of involvement of the phrenic nerves. 09:12 You can have thoracic and back pain. 09:15 And this is related to enlargement of thoracic aorta and impingement on nerve fibers that are coming out of the spine. 09:27 If you have dilation that's near the aortic root, then the aortic valve will dilate, the annulus will dilate and you may have valvular insufficiency. 09:36 So aortic regurgitation with now impressive pressure and volume overload in the left ventricle. 09:44 And this is just demonstrating a very dilated aortic root in the thoracic aorta. 09:49 This could have potentially given rise to aortic insufficiency. 09:57 The other complication that is perhaps most feared is that dilation of the thoracic aorta will give rise to a rupture. 10:08 And with roughly the same statistics, 4-5 cm dilation: 1-2% per year; greater than 5-6 cm: that's going to be about 10% per year; greater than 6 cm: 25% per year. 10:22 The same risk of rupture occurs in the thoracic aorta.
About the Lecture
The lecture Abdominal Aortic Aneurysm and Thoracic Aortic Aneurysm by Richard Mitchell, MD, PhD is from the course Aortic Disease.
Included Quiz Questions
Which of the following is a major risk factor for an abdominal aortic aneurysm?
- Smoking
- Younger age
- Orthostatic hypotension
- Cannabis use
- Long QT syndrome
Which immunoglobulin-related disease is associated with an abdominal aortic aneurysm?
- IgG4-related disease
- IgG3-related disease
- IgG14-related disease
- IgG13-related disease
- IgM14-related disease
What is the most common presentation of a patient with an abdominal aortic aneurysm?
- Asymptomatic
- Abdominal pain
- Nausea
- Syncope
- Leg weakness
What is the risk of rupture of an abdominal aortic aneurysm measuring 4.6 cm in diameter?
- 1% per year
- 45% per year
- 10% per year
- 0.1% per year
- 5% per year
What is the cause of hiccups in a patient with a large thoracic aortic aneurysm?
- Phrenic nerve involvement
- Compression of the trachea
- Compression of the esophagus
- Occlusion of the vasa vasorum
- Mediastinal inflammation
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |