Why Simulation is Essential for Medical and Nursing Education
In today’s clinical landscape, simulation for training is essential to both medical and nursing education. Classroom learning and clinical rotations are foundational, but they frequently lack the repetition, standardization, and safe failure space necessary for mastery. Simulation fills that gap—letting learners rehearse complex clinical scenarios, hone psychomotor and cognitive skills, and receive immediate feedback without risk to patients. This deliberate, feedback-rich practice accelerates skill acquisition across professions and specialties.
“Simulation for training turns theory into reliable performance—without putting patients at risk.”
This article explains the definition and overview of simulation in training, outlines precise types of simulation methods, lists practical simulation training examples, and reviews benefits and challenges—relevant to both medical and nursing faculty. It also spotlights SIMTICS (SimTutor), now part of the Lecturio portfolio, and links to evidence and resources you can use in your curriculum.
Definition and Overview of Simulation in Training
Simulation for training is experiential learning that recreates clinical situations—virtual or in-person—so learners can practice skills, decision-making, and teamwork in a controlled setting. It aligns closely with deliberate practice, which emphasizes focused repetition, coaching, and immediate feedback to improve performance.
For both nursing and medical learners, simulation training in healthcare provides repeat exposure to rare or high-risk cases, allows targeted feedback from instructors or automated systems, and supports progressive skill development that clinical rotations alone may not provide.
Types of Simulation Methods in Training
Different modalities map to different learning goals. Below are precise types of simulation methods in training commonly used across medical and nursing education.
Low-Fidelity Simulation
Task trainers, role-play, or single-skill digital modules for early learners (e.g., IV insertion, basic wound care). Ideal for foundational practice.
High-Fidelity Simulation
Advanced manikins and staged clinical environments that mimic emergencies (e.g., cardiac arrest, trauma). Common for both simulation training for nurses and simulation training for doctors to develop teamwork and procedural competence.
Virtual Reality (VR) & Augmented Reality (AR)
Immersive environments for virtual reality simulation training for student nurse education and medical procedural practice—allowing repeatable, asynchronous practice across distributed learners.
Standardized Patients
Actors trained to portray clinical cases for realistic practice of communication, history-taking, and diagnostic reasoning.
Hybrid Simulation
Combines manikins, standardized patients, and digital modules to balance realism and repeatability.
Rapid-Cycle Deliberate Practice (RCDP)
Short, iterative cycles: stop for targeted feedback, then restart to reinforce correct behaviours. RCDP has demonstrated improvements in team performance and individual skills in high-stakes settings.
Benefits of Simulation for Learners
Simulation-based learning in medical education and nursing programs demonstrates multiple clear benefits:
- Safe environment: practice without patient risk;
- Deliberate repetition: practice until reliable performance;
- Immediate feedback: correct errors faster;
- Bridging theory and practice: apply classroom knowledge to realistic clinical scenarios;
- Standardization: comparable assessments across learners;
- Interprofessional learning: teams train together to improve communication and safety.
Programs combining simulation with deliberate practice have shown measurable reductions in errors and meaningful improvements in clinical performance—demonstrating direct impact on patient safety. For example, a simulation- and deliberate practice-based program reduced interns’ errors in blood-product requests by ~65% compared to untrained peers.
Practical Examples of Simulation in Healthcare
Simulation is now central across many curricular areas. Representative simulation training examples include:
- Trauma resuscitation practice using RCDP with high-fidelity manikins for surgical residents and interdisciplinary teams.
- Airway and patient deterioration scenarios for nursing students using hybrid simulation approaches.
- Virtual patient cases for diagnostic reasoning practice in both medical and nursing programs.
- Faculty development workshops that train educators in debriefing, assessment, and simulation design.
Training and Simulation for Patient Safety
Training and simulation for patient safety provides a systematic way to identify and close performance gaps before learners enter real clinical care. Evidence shows simulation-based deliberate practice improves team coordination and decreases harmful errors—making it one of the most effective educational strategies for improving patient outcomes.
Challenges and Limitations of Simulation Training
Simulation is powerful but has constraints that educators should address when planning programs:
- Resource demands: high-fidelity labs, VR hardware, and ongoing maintenance cost money;
- Faculty development: scenario design and debriefing require instructor training;
- Scalability: physical labs limit large-cohort access unless augmented by web-based simulation;
- Transfer to clinical practice: simulation gains require reinforcement for durable transfer;
- Learner perception: authenticity and psychological safety influence effectiveness.
Blended approaches, scalable digital modules, and structured faculty development are practical strategies to mitigate these barriers.
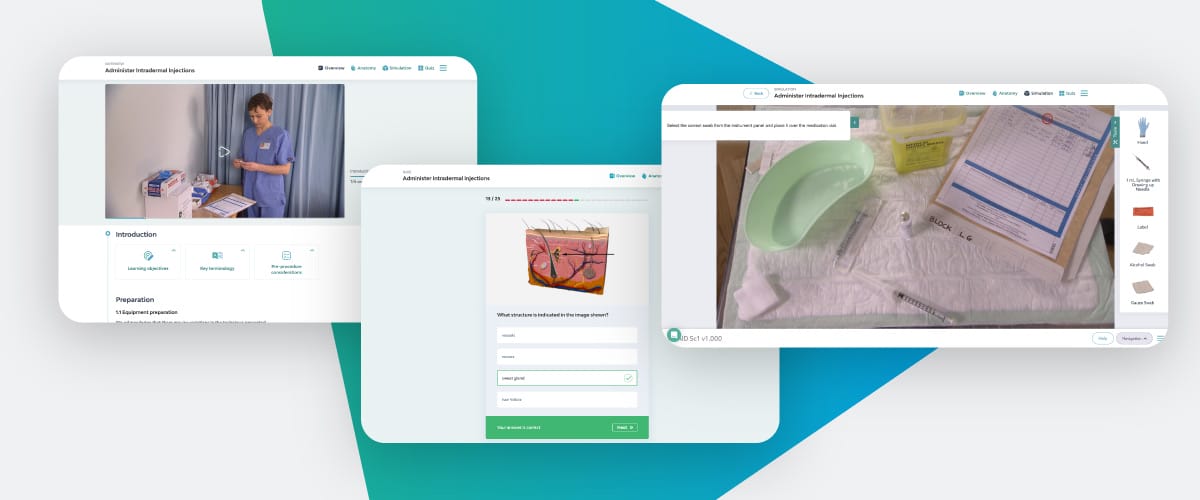
Spotlight: SIMTICS & SimTutor — Now Part of Lecturio
SIMTICS expands access to repeatable, web-based simulation modules for both nursing and medical programs.To scale simulation training across distributed or large cohorts, web-based solutions are essential. SimTutor’s SIMTICS is a browser-based platform with a library of 200+ interactive modules—procedural walkthroughs, 3-D anatomy, quizzes, and guided simulation steps—designed for repeatable, asynchronous practice.