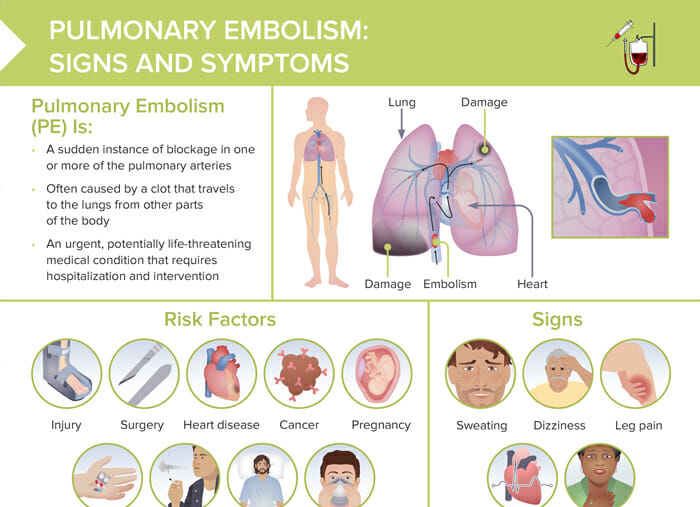
What is a pulmonary embolism?
A pulmonary embolism is a sudden instance of blockage in one or more of the pulmonary arteries, often caused by a clot that travels to the lungs from other parts of the body. Pulmonary embolisms are an urgent, potentially life-threatening medical condition that requires hospitalization and intervention.
What can cause pulmonary embolism?
Factors that increase the risk of pulmonary embolism include:
- Injury
- Surgery
- Heart disease
- Cancer
- Pregnancy
- Supplemental estrogen
- Smoking
- Prolonged immobility
- COVID-19
Signs of pulmonary embolism
Signs of pulmonary embolism include:
- Sweating
- Dizziness
- Leg pain
- Irregular heartbeat
- Shortness of breath
How to assess for pulmonary embolism: what is the best diagnostic test?
PE mimics several other health conditions and is often overlooked in clients who might have similar symptoms. Thorough assessment and monitoring of sudden changes in signs, intake and output, edema, or breathing patterns is essential.
If PE is suspected, diagnostic testing often involves imaging, such as a chest X-ray, ultrasound, MRI, pulmonary angiogram, ventilation-perfusion scan (V/Q scan), and bloodwork.
Pulmonary embolism nursing care plan (example)
Examine the contents of a care plan for an example client (who received a pulmonary embolism diagnosis after presenting with symptoms of shortness of breath and chest pain) could look like (nursing diagnoses, objective, and interventions). At the end, the evaluation of the actions taken should follow, documenting how the client responded to the planned interventions.
Assessment:
Subjective and objective data: dyspnea with respirations at 24/min, headache, confusion, tachycardia
Potential nursing diagnosis:
Potential nursing diagnoses for a pulmonary embolism can include:
- Impaired gas exchange related to alveolar-capillary membrane changes (embolic obstruction)
- Decreased cardiac output related to right ventricular failure secondary to acute pulmonary hypertension
- Acute pain related to decreased myocardial oxygenation
- Impaired spontaneous ventilation related to decreased lung compliance & increased work of breathing
- Activity intolerance related to oxygen supply/demand imbalance
- Risk for shock related to potential right-sided heart failure
Planning:
Addressing the planning phase of the care plan for impaired gas exchange:
- “Within the next 24 hours, the patient will demonstrate improved gas exchange as evidenced by SpO2 levels greater than 94% on room air, normal respiratory rate, and absence of dyspnea.”
- Anticoagulation medication. If a client cannot be anticoagulated, a vena cava filter may be considered.
Note: Educate patients that anticoagulants will be taken for an extended period of time.
Interventions:
- Respiratory monitoring:
- To address impaired gas exchange and impaired spontaneous ventilation
- Assess respiratory rate, rhythm, and depth.
- Monitor oxygen saturation using pulse oximetry.
- Listen to lung sounds regularly for changes or abnormalities.
- Oxygen therapy: Administer supplemental oxygen to address impaired gas exchange.
- Cardiac monitoring:
- To address risk for shock and decreased cardiac output
- Monitor heart rate and rhythm through telemetry or ECG.
- Assess for signs of right-sided heart strain or failure, which can be a complication of a massive PE.
- Pain management
- Leg exercises:
- To address activity intolerance
- Encourage leg exercises to promote venous return and prevent deep vein thrombosis.
- Assist with early ambulation as tolerated and prescribed.
- Patient education
Evaluation:
Educate client/family on medication adherence and adverse effects. Emphasize regular monitoring of blood parameters for medication dose.
How long before a pulmonary embolism is fatal?
Factors influencing the mortality of pulmonary embolism, and how quickly a patient can deteriorate, include:
- Size of the embolism
- Overall health status of the client
- Presence of deep vein thrombosis (additional clots)
- How promptly treatment is initiated
- Right ventricular failure
How long can a pulmonary embolism be present without symptoms showing?
If symptoms are mild, an affected person might not immediately notice they are experiencing a pulmonary embolism – in some cases, for hours or days, or even longer. Factors that can influence this include:
- Smaller clots might not cause noticeable symptoms
- Slowly-developing embolisms may cause symptoms that develop gradually and may be dismissed
- Symptoms can be nonspecific and not be assigned to a pulmonary embolism, but potential coexisting conditions
What is a saddle pulmonary embolism?
A saddle pulmonary embolism refers to a large blood clot that straddles the bifurcation (or split) of the main pulmonary artery into the left and right main pulmonary arteries. This positioning resembles a saddle, which is where the term comes from.