The trend-item materials
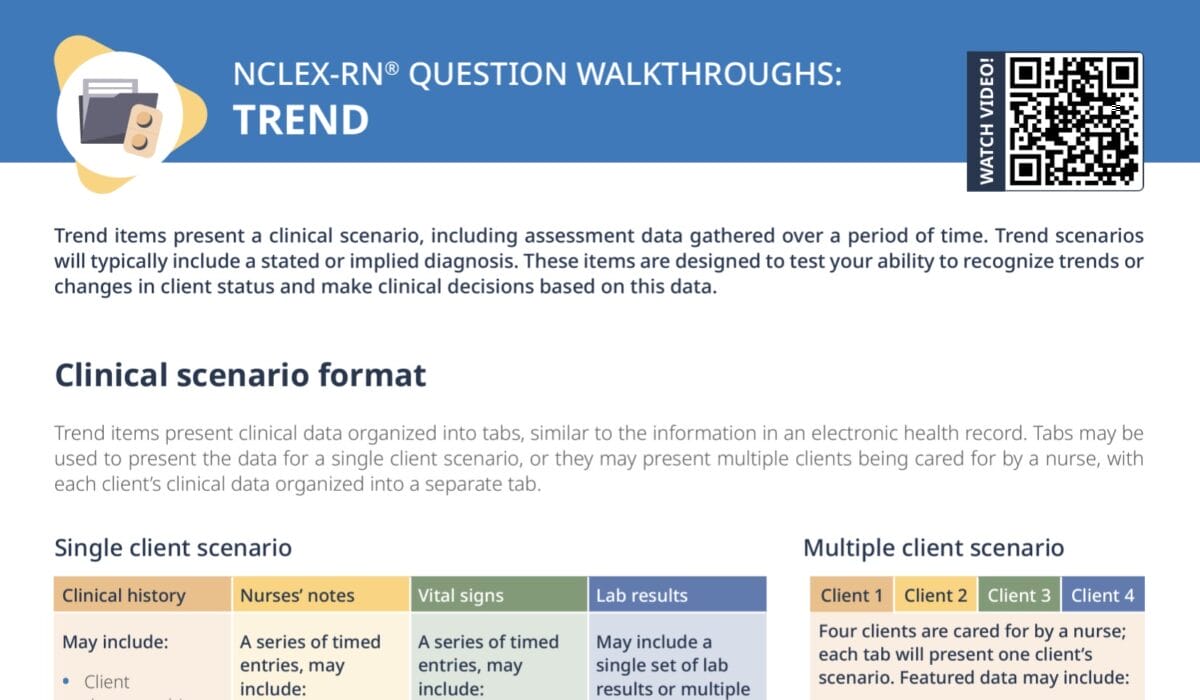
While a lot of questions that focus on prioritization are standard single–choice questions, they can also come in the form of trend items. In these, the question is paired with a clinical scenario presented in the form of several tabs filled with information. You review this information and base your answer choice on the developments over time you infer from it.
Tab 1: Tuesday, 0800–0830
Client 1:
A 37-year-old client who sustained a motor vehicle accident the previous day. The client has no visible injuries on the body other than some abdominal bruising and pain, but reports feeling “weak.”
Client 2:
An 82-year-old client with suspected food poisoning who has vomited 4 times today. The family reports that the client seems confused.
Client 3:
A 6-month-old infant with increased drooling and rash on the lip/chin area. The mother states that the infant has been more irritable than usual.
Client 4:
A 60-year-old client who had a cholecystectomy 6 days ago and reports severe pain at the surgical site
Tab 2: Tuesday, 1000–1030
Client 1:
The client has developed abdominal distension and dizziness.
Client 2:
The client has vomited 2 more times and is not oriented to place.
Client 3:
The client feels very warm to the touch.
Client 4:
There is a yellowish, purulent discharge at the surgical site.
Tab 3: Vital signs
| Client 1 | Client 2 | Client 3 | Client 4 | |
| HR | 107/min | 110/min | 160/min | 97/min |
| BP | 82/40 mm Hg | 92/50 mm Hg | 88/63 mm Hg | 148/92 mm Hg |
| RR | 26/min | 20/min | 58/min | 22/min |
| T | 96.8°F (36°C) | 99.6°F (37.7°C) | 100°F (37.9°C) | 100.4°F (38°C) |
| Pulse ox | 94% | 96% | 98% | 98% |
Play out the scenario for each client: tab 1
Staying in the first tab, ask yourself: What is the worst case scenario for each client?
Prioritize accordingly, if already possible. If not, that’s okay, this first tab will just be your baseline. Then, move on to the next tab with the later assessments and recheck your prioritization, or note the development of each client. Is anyone rapidly deteriorating? Is anyone showing signs of a much more serious condition than you originally thought and needs immediate attention? This is where you will get the clues that guide your prioritization.
Client 1 at 0800–0830
This client is 37 years old and was in a motor vehicle accident yesterday. Assessment findings include abdominal bruising and pain, and feeling “weak.”
Client 2 at 0800–0830
This client’s age, 82, is at first glance more concerning, since it is an elderly person. The repeated vomiting –suspected to be due to food poisoning– would cause this client to be dehydrated, which can cause confusion especially in older clients.
Client 3 at 0800–0830
The infant is 6 months old, irritable, drooling more than usual, and has a rash on the lip/chin area. At 6 months old, a possible explanation for this child’s presentation could be cutting teeth, during which drooling and irritation would be normal and not a special concern.
Client 4 at 0800–0830
At 60 years old, this client is older, but not quite elderly yet. Severe pain at the surgical site when the gallbladder was removed 6 days ago (cholecystectomy) would not be considered normal.
Look at how each client develops: tab 2
Client 1 at 1000–1030
This client’s weakness has evolved into dizziness, and the new assessment is abdominal distention. With the assumed trauma in the MVA the client experienced the day before, the bruising, and how their symptoms developed, keep in mind any potential problems that could occur.
Client 2 at 1000–1030
The client lost orientation to place after having vomited twice more, which indicates the dehydration has worsened.
Client 3 at 1000–1030
The client feeling warm could indicate fever, but with the other signs and this being the only addition, the suspicion that the infant is just cutting teeth is reaffirmed. They would probably not need any priority care at this time.
Client 4 at 1000–1030
Yellowish, purulent discharge at the surgical site suggests an infection as the cause of the client’s intense pain.
Vital signs: tab 3
As always, when you are given numerical values, judge them: Is this low, normal, or high?
Client 1
- HR 107/min: fast
- BP of 82/40: very low!
Client 2
- HR 110/min: a bit high, blood pressure a bit low, normal pulse ox
- RR 20: lower than in client 1 and slightly elevated temperature
Client 3
- HR 160/min: would be of concern for an adult, but for the infant it is not as much of a problem
- Temperature 100°F: a bit warm
- RR 58: Fast breathing but pulse ox 98%
Client 4
- 148/92 mm Hg: High
- RR 22: On the upper end
- Temperature 100.4°F: slightly elevated
- Pulse ox normal
Compare by client over time and prioritize according to their “trend”
In trend items like this one, it can be easy to get overwhelmed and lose the way between the different tabs, time stamps, and clients. A trick to stay focused is to follow each client through the timeline separately: Client 1 presents with X, then develops into Y. Client 2 presents with X, and Y and Z happen a bit later. And so on. This way, you sort the information into exactly what you will need to compare to prioritize.
This means you will click through the tabs several times, following one client each time to look at the entire timeline of this client. Then, you repeat for the next client and compare: Is this client more or less unstable as the other one?
Client 3
This child has no concerning respiratory issues and the symptoms can be explained with teething. So, this infant is not going to be the most urgent priority when compared to the other serious cases that include a trauma victim and a dehydrated elderly client, that can be expected to be a lot less stable. → eliminate answer
Client 4
This client very likely is experiencing a postoperative infection at the surgical site; suspected based on the pain, the fever, and the discharge from the site. Looking at this client’s vital signs, while they definitely will need treatment for the infection, they are not acutely as unstable as either the trauma case or the elderly client with dehydration. → eliminate answer
Client 2
Dehydration is confirmed by the repeated vomiting, the disorientation, the high heart rate and the low blood pressure. The fluids definitely need to be replaced, but when comparing this case of hypovolemia to a case where it is caused by abdominal hemorrhage, this client is still more stable at the moment. → eliminate answer
Client 1
With MVAs, there is a risk of bleeding, of which bruising is a sign. So, for this client, there is a suspicion of abdominal hemorrhage. The client’s symptoms support a suspicion of hypovolemia (weak, dizzy, low blood pressure, high heart rate), which supports the suspicion of abdominal hemorrhage further. The worst case scenario for this would be the client going into shock. Compared to the other three clients, this client is the most unstable and the person who is at the highest immediate risk. Treatment of this client should therefore take top priority. → correct answer